Featured Papers
Influence of Body Size with Increased BMI on the Risk of Metabolic and Cardiovascular Diseases
Impact of higher BMI on cardiometabolic risk: does height matter?
Lancet Diabetes Endocrinol 2024
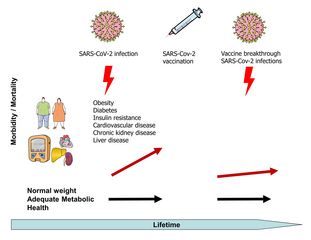
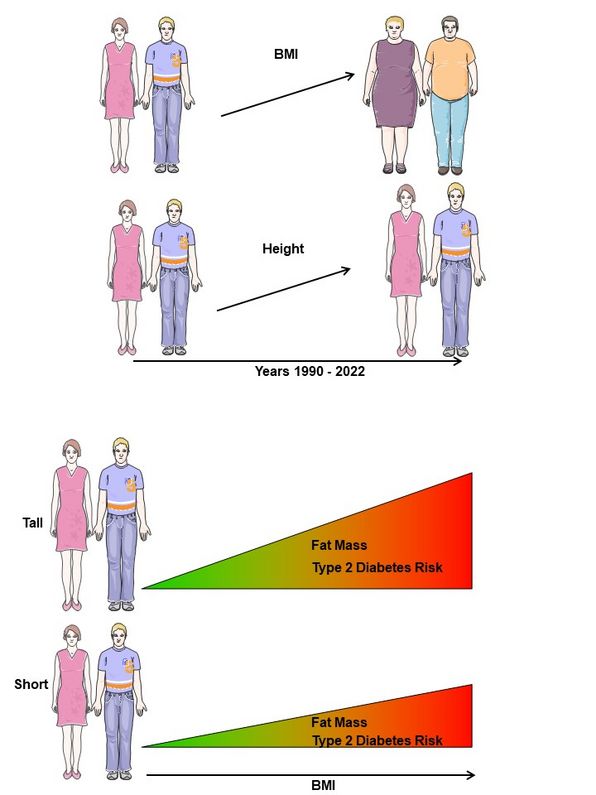
If the body mass index (BMI) is the only factor used as a basis for tall people, the risk of type 2 diabetes and cardiovascular disease might be underestimated. Studies by the German Center for Diabetes Research (DZD) indicate that the fat level and the risk of type 2 diabetes are higher in larger people than in smaller people even if the increase in their BMI is the same. The results of their examinations have now been published in “The Lancet Diabetes & Endocrinology”.
Since 1990, four times more children and adolescents have become obese (as measured by the BMI) and adult obesity rates have more than doubled. This development is strongly associated with an increased risk to BMI-related diseases such as cardiovascular disease and type 2 diabetes. At the same time, people have grown taller in recent decades.
Does body height increase the meaningfulness of the BMI?
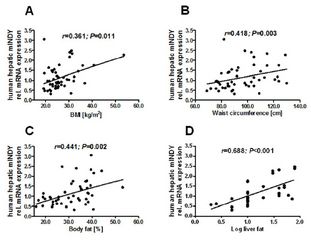
“The BMI is merely an approximation for determining the body fat level,” explains Norbert Stefan from DZD partner Helmholtz Munich and the University of Tübingen. “It is not yet known whether an increased body height changes the BMI meaningfulness as a measure of body fat level and cardiometabolic risk,” adds Matthias Schulze from the German Institute of Human Nutrition Potsdam-Rehbrücke, another DZD partner. To examine this question, the researchers analyzed the data of 972 people aged 18 years and older who took part in the Tübingen Diabetes Family Study. Their fat mass was determined using whole-body MRI. This showed that the positive correlation between BMI and accurately measured total body fat mass becomes stronger with increasing body height in both women and men. This correlation was neither influenced by age nor by the volume of the skeletal muscles of the upper and lower body. In a further analysis of data from 25,393 participants in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study, the researchers found that the risk of type 2 diabetes gradually increased with a BMI increase of 5 kg/m² from 1.58 in the lowest height category (≤150 cm) to 2.85 in the highest height category (>180 cm).
Higher type 2 diabetes risk with increased BMI: larger people more affected than smaller ones
The results suggest that the BMI better reflects fat mass and cardiometabolic risk in larger people than in smaller people. The researchers also suspect that today's adults may be exposed to a higher BMI-related health burden compared to historical populations due to their larger body size. It is therefore important to take into account the increase in body size that has occurred in recent decades in order to better estimate the burden of cardiometabolic disease due to obesity in the future.
© Norbert Stefan
Original publication:
Stefan N, Schiborn C, Machann J, Birkenfeld AL, Schulze MB. Impact of higher BMI on cardiometabolic risk: does height matter? Lancet Diabetes Endocrinol 2024. Published Online July 2, 2024, doi.org/10.1016/S2213-8587(24)00164-5
Biomarkers Indicate Damage to Nerves
Associations between multiple neurological biomarkers and distal sensorimotor polyneuropathy: KORA F4/FF4 study.
Diabetes/Metabolism Research and Reviews 2024
Damage to the peripheral nervous system, referred to as polyneuropathy, is a common complication of diabetes which is often diagnosed at a late point only. In the journal “Diabetes/Metabolism Research and Reviews,” researchers from the DZD report on the identification of biomarkers that can be measured in the blood and are associated with distal sensorimotor polyneuropathy.
Distal sensorimotor polyneuropathy (DSPN) is the most common polyneuropathy in people with type 2 diabetes. However, it can also develop in people without manifest diabetes. Older age, obesity, prediabetes and dyslipidemia have emerged as risk factors. Characteristic symptoms are pain, paresthesia (burning, tingling), but also numbness, unsteady gait or muscle weakness.
Analysis of more than 1,000 blood samples
Researchers from the German Diabetes Center (DDZ) in Düsseldorf, in collaboration with researchers from the German Center for Diabetes Research (DZD) at Helmholtz Zentrum München and with partners from other institutions, have now been able to show that specific biomarkers can be detected in higher concentrations in the blood of DSPN patients than in people without DSPN. They analyzed blood samples from 1,032 participants in the KORA study. KORA examines the state of health of the population in Augsburg and the surrounding area. 177 study participants already had DSPN at the start of the study.
Of 88 biomarkers examined, 2 were associated with DSPN: the proteins CTSC and PDGFRα. People with high CTSC and PDGFRα levels were particularly likely to have DSPN. This applied to study participants with and without type 2 diabetes.
Association only with pre-existing polyneuropathy
In addition, 5 other biomarkers (CDH3, JAM-B, LAYN, RGMA and SCARA5) were positively associated with DSPN in people with diabetes, who made up one-fifth of the study cohort. The biomarker GCP5 was associated with DSPN in people without diabetes only.
Some of the participants in the KORA study did not develop DSPN until several years into the study. However, the researchers were unable to observe an association between the biomarkers examined and the recurrence of the disease.
Often, DSPN is recognized only at a very late point. If they confirm their significance in further studies, the biomarkers identified could be used for screening, for example – to detect the disease earlier and monitor its progression. It is possible that CTSC and PDGFRα are also involved in the development of DSPN. They would then be potential working points for the development of new drugs.
Original publication:
Christian Herder, Barbara Thorand, Alexander Strom, Wolfgang Rathmann, Margit Heier, Wolfgang Koenig, Helen Morrison, Dan Ziegler, Michael Roden, Annette Peters, Gidon J. Bönhof und Haifa Maalmi. Associations between multiple neurological biomarkers and distal sensorimotor polyneuropathy: KORA F4/FF4 study. Diabetes/Metabolism Research and Reviews 2024
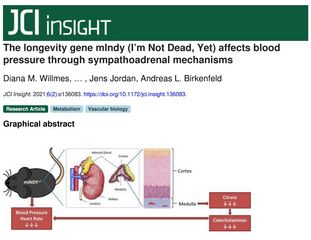
Polyagonists Enable Increasingly Effective Treatment of Obesity and Diabetes
Dual and Triple Incretin‑Based Co‑agonists: Novel Therapeutics for Obesity and Diabetes.
Diabetes Therapy 2024
The drug semaglutide, a GLP-1 receptor agonist, was developed for the treatment of type 2 diabetes (T2D). However, it is also currently widely discussed as a “slimming injection”. Polyagonists that combine several hormones achieve even more impressive results in the treatment of obesity and T2D. With dual and triple agonists, clinical studies are now achieving results that are otherwise only known from bariatric surgery. In the “Diabetes Therapy” journal, researchers from the DZD and Helmholtz Munich provide an overview of these new diabetes and obesity drugs.
More and more people around the world are suffering from obesity and/or type 2 diabetes. New effective treatment options are urgently needed. The discovery of long-acting incretin receptor agonists was a major step forward.
Incretins are hormones produced in the intestine that regulate the release of the blood sugar-lowering hormone insulin during food intake. By inhibiting the insulin antagonist glucagon, they also stimulate the satiety center in the brain. Synthetic incretin receptor agonists are similar to natural incretins and can mimic their effect.
Researchers from the German Center for Diabetes Research (DZD) and Helmholtz Munich, in collaboration with a colleague from the University of Santiago de Compostela in Spain, describe the development of incretin-based pharmacotherapy from its beginnings to the discovery of polyagonists. According to the group of authors, these polyagonists are “in all likelihood the next step towards a cure for diabetes and obesity.”
Comparable to bariatric surgery
The authors report on various polyagonists that are currently being researched in clinical studies and “show improved efficacy with each new generation.” The latest triple agonists attack both the glucose-dependent insulinotropic peptide receptor (GIPR) and the receptors for glucagon-like peptide 1 (GLP1) and glucagon (GCG, a hormone from the pancreas). According to the study reports, their effect can rival that of bariatric surgery – both in terms of treating diabetes and obesity.
Nevertheless, the authors warn against too much euphoria, as there are still some challenges ahead. For example, it is not yet fully understood how incretin receptor agonists achieve their effect on body weight. The safety profile of the new drugs also still needs to be improved, as does patient access to the new therapies.
Original publication:
Robert M. Gutgesell, Rubén Nogueiras, Matthias H. Tschöp, Timo D. Müller. Dual and Triple Incretin‑Based Co‑agonists: Novel Therapeutics for Obesity and Diabetes. Diabetes Therapy 2024 Apr 4; doi: 10.1007/s13300-024-01566-x
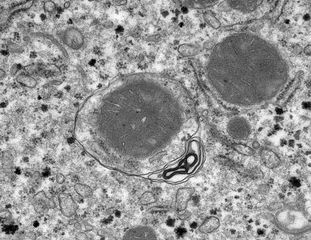
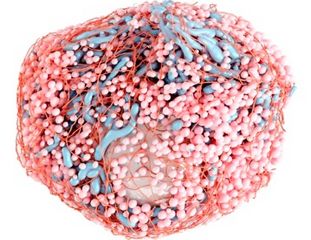
Novel Protocol Advances 3D Electron Microscopy Analysis
Modular segmentation, spatial analysis and visualization of volume electron microscopy datasets.
Nat Protoc. 2024
Volume electron microscopy is currently revolutionizing our knowledge of cells and tissues by enabling structural imaging in 3 dimensions. Now, researchers from the Paul Langerhans Institute Dresden (PLID) of the German Center for Diabetes Research have introduced a novel protocol designed to transform the analysis of three-dimensional electron microscopy (3D-EM) datasets. In collaboration with colleagues from the Max Delbrück Center for Molecular Medicine (MDC), the Humboldt-University Berlin, Helmholtz Imaging and the École Polytechnique Fédérale de Lausanne (EFPL) the scientists developed detailed guidelines, aimed at imaging scientists in biology and medicine, offering a modular and user-friendly workflow to unravel the intricate details of cellular ultrastructure. This new protocol has now been published in the renowned journal “Nature Protocols”.
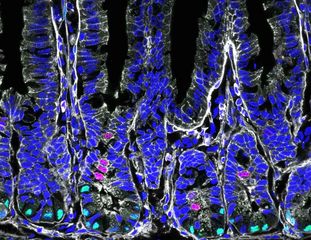
For decades, two-dimensional electron microscopy has been the cornerstone of cell biology and medical research, providing detailed insights into subcellular components. In recent years, the surge in three-dimensional volume electron microscopy (vEM) methods has led to an abundance of large raw image datasets, necessitating advanced analysis approaches. The newly developed protocol addresses this demand by providing comprehensive procedures for raw data preparation, organelle-specific segmentation, spatial analysis of segmentation maps, and 3D visualization.

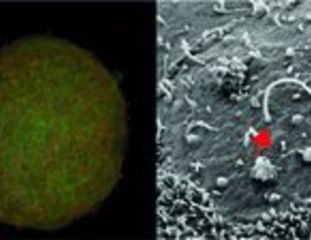
© PLID
Andreas Müller, senior scientist at the PLID and first author of the article elucidates the motivation behind the protocol, stating, “Our aim was to simplify the challenges researchers face when analyzing complete cells in vEM datasets. These datasets are huge and segmentation of the cellular features is very time-consuming. Also, although there are a lot of different software tools available to help with this, not all of them are user-friendly and straight-forward to apply."
The protocol's modular approach stands out as a key feature, offering a versatile framework for vEM analysis. Researchers can choose from a variety of segmentation methods tailored to specific organelles, reducing unnecessary annotation effort, and expediting early project results. Müller emphasizes the adaptability of the workflow, noting, "While the initial project for which we designed the workflow was on pancreatic beta cells, the segmentation, analysis, and rendering workflows are designed to easily adapt to other cell types and vEM modalities."
The advantage of the new protocol is its accessibility to imaging scientists with medium-level computational expertise. The protocol encourages users to incorporate their preferred segmentation tools, providing a streamlined process through “Album” solutions. “Album is a platform that we developed to make complex analysis pipelines easier to distribute and use in a reproducible way.” says Deborah Schmidt, head of the Helmholtz Imaging Solutions Team at MDC and co-first author of the article. This innovative methodology is poised to accelerate advancements in cellular biology, offering a clearer understanding of cellular ultrastructure. Martin Weigert, research group leader at the EFPL and senior author of the protocol summarizes the significance of the protocol, stating, "Our protocol provides an extensive overview of time- and labor-efficient solutions for vEM analysis and should serve as a useful reference for the broader vEM research community."
In summary, this pioneering protocol by Andreas Müller and his co-workers marks a significant stride towards democratizing access to 3D-EM methodologies, fostering collaboration and advancing the frontiers of cellular research.
Original publication:
Müller A, Schmidt D, Albrecht JP, Rieckert L, Otto M, Galicia Garcia LE, Fabig G, Solimena M, Weigert M. Modular segmentation, spatial analysis and visualization of volume electron microscopy datasets.Nat Protoc. 2024 Feb 29. doi: 10.1038/s41596-024-00957-5.
Potential Novel Biomarkers of Coronary Heart Disease Discovered
Association of plasma proteomics with incident coronary heart disease in individuals with and without type 2 diabetes: results from the population-based KORA study.
Cardiovasc Diabetol 2024
Coronary heart disease is a major global health problem, especially among people with type 2 diabetes. Researchers at the German Center for Diabetes Research (DZD), Helmholtz Munich, and Ludwig-Maximilians-University Munich (LMU) have identified novel protein biomarkers that are associated with the development of CHD in people with and without diabetes. The results have been published in ‘Cardiovascular Diabetology.’
Coronary heart disease (CHD) is one of the most common causes of death worldwide—especially in Europe: Here, it is responsible for nearly half of all deaths. Among middle-aged adults, individuals with type 2 diabetes (T2D) have a two to four times higher risk of developing CHD than people without T2D. The research team investigated the predictive performance of protein biomarkers on incident CHD in individuals with and without T2D.
For their study, the researchers used data from Cooperative Health Research in the Region of Augsburg (KORA). The validation cohort included 888 participants from the KORA-Age1 study with 70 incident cases of CHD (19 vs. 51 cases in the group with T2D and without T2D, respectively) during 6.9 years of follow-up. They tested blood samples of the subjects for 233 plasma proteins related to cardiovascular disease and inflammation.
The researchers thus identified two proteins associated with incident CHD in individuals with diabetes and 29 proteins in those without baseline T2D. Six of these proteins are novel candidates for incident CHD.

© Helmholtz Munich
The results of this study contribute significantly to a better understanding of the pathophysiology of CHD in T2D patients and offer potential new approaches to the prevention and treatment of this serious complication. They underscore the importance of further research in this area and the role of the German Center for Diabetes Research in resolving pressing issues related to diabetes and its complications.
Original publication:
Luo, H., Huemer, MT., Petrera, A. et al. Association of plasma proteomics with incident coronary heart disease in individuals with and without type 2 diabetes: results from the population-based KORA study. Cardiovasc Diabetol 23, 53 (2024). https://doi.org/10.1186/s12933-024-02143-z
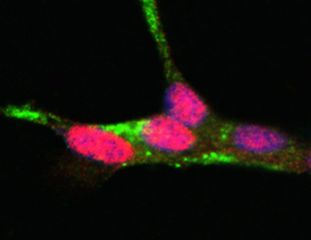
Regenerative Medicine: Increased Availability of Pancreatic Progenitor Cells
Regulation of multiple signaling pathways promotes the consistent expansion of human pancreatic progenitors in defined conditions.
Elife 2024
Researchers at the DZD partner Paul Langerhans Institute Dresden have identified mechanisms that promote the expansion and differentiation of pancreatic progenitor cells (PP). In future, these mechanisms could support the unlimited expansion of human pluripotent stem (hPS) cell-derived PP cells. The results, published in “Elife”, set the stage for new ways of treating diabetes.
Nearly ten percent of the world's population has diabetes and, in severe cases, treatment requires whole pancreas transplantation or the transplantation of insulin-producing islet cells. However, the widespread application of this approach to treating diabetes is currently limited by a scarcity of organ donors. Furthermore, affected individuals require lifelong medications that suppress the immune system so that the body does not reject the transplanted organs. Therefore, scientists at the DZD are working on utilizing human pluripotent stem (hPS) cells for the generation of insulin-producing cells.
Chemically Optimized Expansion Medium Decouples PP Proliferation from Differentiation
The team led by Prof. Anthony Gavalas at the Paul Langerhans Institute Dresden has already made significant progress in the expansion of hPS cell-derived progenitors. According to their recently published results, the greatest challenge lay in maintaining the self-renewal of PP cells while simultaneously inhibiting their differentiation. The chemically optimized cell culture medium decouples the proliferation of PP cells from their differentiation and enables up to a 2000-fold expansion over 10 passages and 40–45 days, without impairing differentiation.

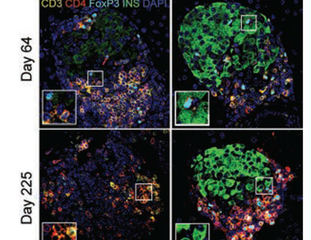
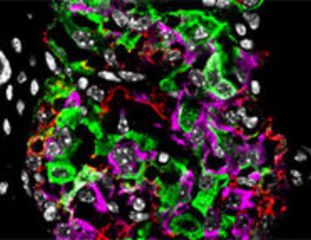
Representative images of immunofluorescent staining of p0 PP cells as well as C5-expanded cells at p5 and p10 for the PP transcription factors PDX1, NKX6.1, and SOX9. © PLID
A Highly Promising Outlook: The Method is Scalable
The method is versatile and scalable. The researchers have patented the procedure and entered into an agreement for commercial development.
This pioneering work marks an important milestone on the path to more effective diabetes treatments and demonstrates the potential of regenerative medicine.
Original publication:
Jarc L, Bandral M, Zanfrini E, Lesche M, Kufrin V, Sendra R, Pezzolla D, Giannios I, Khattak S, Neumann K, Ludwig B, Gavalas A. Regulation of multiple signaling pathways promotes the consistent expansion of human pancreatic progenitors in defined conditions. Elife. 2024 Jan 5;12:RP89962. doi: 10.7554/eLife.89962.
Does Metformin Influence Brain Development? Research Data from a Study with Mice
Developmental metformin exposure does not rescue physiological impairments derived from early exposure to altered maternal metabolic state in offspring mice.
Molecular Metabolism 2023
The number of women who develop gestational diabetes during pregnancy has been increasing for years. Drugs used to treat diabetes, such as metformin, cross the placental barrier. In the specialist journal Molecular Metabolism, researchers report on a study with mice, in which metformin had an impact on offspring brain development—how exactly was dependent on the metabolic state of the mother.
The hypothalamus region of the brain plays a key role in regulating energy homeostasis. In mice, neuronal connectivity in the hypothalamus is established during the first postnatal weeks. This is a critical time window, during which antidiabetic treatment could lead to changes. For example, the diabetes drug metformin has an impact on the AMPK enzyme, which regulates axonal growth during brain development.
High-Fat or Control Diet
Researchers from the German Institute of Nutritional Research Potsdam-Rehbrücke (DIfE), Nuthetal, the German Center for Diabetes Research (DZD), Munich/Neuherberg, and the Charité- Universitätsmedizin Berlin investigated how metformin treatment and the metabolic state of the mother impact the physiology and brain development of young animals.
For the study, female mice received either a control diet or a high-fat diet before mating and during pregnancy and lactation periods. Obesity and excessive weight gain during pregnancy are the main risk factors for gestational diabetes. The mice that were fed a high-fat diet developed symptoms of a metabolic disorder and were hyperglycemic at the end of the lactation period.
Metformin During the Brain Development Period
During the first three postnatal weeks, both the mothers and offspring received metformin. Gestational diabetes is usually diagnosed between the 24th and 28th week of pregnancy and medical treatment is provided during the third trimester. With regard to brain development, the lactation period in rodents corresponds to the third trimester of a human pregnancy.
Metformin treatment had measurable but variable impacts on the weight and hormones of the offspring. The researchers also observed effects on various components of the AMPK signaling cascade in the developing hypothalamus of the young mice. These were influenced by the metformin treatment as well as the diet given to the mother and the sex of the offspring.
The scientists explain that early changes in the hypothalamus could predispose the offspring to metabolic disorders later in life. In future studies, the young animals could be observed until adulthood in order to better understand the long-term effects of metformin treatment.
Original publication:
Lídia Cantacorps, Jiajie Zhu, Selma Yagoub, Bethany M. Coull, Joanne Falck, Robert A. Chesters, Katrin Ritter, Miguel Serrano-Lope, Katharina Tscherepentschuk, Lea-Sophie Kasch, Maya Paterson, Paula Täger, David Baidoe-Ansah, Shuchita Pandey, Carla Igual-Gil, Annett Braune, Rachel N. Lippert. Developmental metformin exposure does not rescue physiological impairments derived from early exposure to altered maternal metabolic state in offspring mice. Molecular Metabolism 2023 Dec 23; doi: 10.1016/j.molmet.2023.101860.
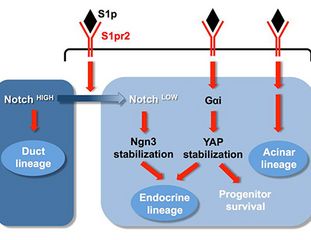
Neurogenin-3 in Pancreatic Cells: Even Low Expression May Prevents Diabetes
Integrating single-cell imaging and RNA sequencing datasets links differentiation and morphogenetic dynamics of human pancreatic endocrine progenitors.
Developmental Cell 2023
In the human embryo, the endocrine cells of the islets of Langerhans develop from epithelial pancreatic progenitor cells. Transcription factor neurogenin-3 is crucial for differentiation. Only with its help can insulin-producing beta cells develop. Neurogenin-3 gene mutations lead to diabetes. Researchers developed a technique to observe neurogenin-3 gene expression in human pancreatic cells. They discovered that even a weak expression enables beta cell formation to prevent the onset of diabetes.
The islets of Langerhans in the pancreas contain various endocrine cells that produce hormones essential for carbohydrate metabolism regulation. While beta cells produce the blood sugar-reducing hormone insulin, alpha cells, for example, produce its counterpart glucagon.
Neurogenin-3 Essential for Differentiation
During the pancreas development phase, transcription factor neurogenin-3 ensures the differentiation of these endocrine cells from the epithelial progenitor cells of the pancreas. For this reason, the highest neurogenin-3 concentration is found in the early phase of organogenesis with a significant reduction occurring before birth. The adult pancreas contains almost no neurogenin-3.
Researchers at the Max Planck Institute of Molecular Cell Biology and Genetics in Dresden and the DZD partner Paul Langerhans Institute Dresden of the Helmholtz Zentrum München at the University Medical Center Carl Gustav Carus of the TU Dresden, and the Novo Nordisk Foundation at the University of Copenhagen, studied how neurogenin-3 behaves in individual cells.
Weak Expression Is Sufficient
They developed 2- and 3-dimensional models using young human pancreatic cells in which they could localize neurogenin-3 using special markers. They discovered that the neurogenin-3 gene is expressed differently in the various pancreatic cells. Some cells display a strong expression and others only a weak expression. The researchers were surprised to find that despite the varying expression strengths, all pancreatic cells were endocrine active and producing hormones.
Apparently, even small amounts of neurogenin-3 are sufficient to trigger endocrine cell differentiation, e.g., beta cell development. According to the researchers, this is important as it explains why neurogenin-3 gene mutations with a small effect on activity do not result in the onset of diabetes in humans. Only mutations causing severe gene impairment lead to diabetes.
Beta Cell Development Requires Time
A further discovery was the fact that neurogenin-3 works slower in humans than in mice. For the researchers, this is evidence that the gene requires more time in humans to fulfill its tasks. Epithelial progenitor cells differentiating into beta or alpha cells take twice as long in humans as in rodents.
The cell culture systems the researchers developed help to better understand how cells develop organs in human embryos. The observation of neurogenin-3 in individual cells demonstrates how the activity of certain genes during embryonic development can lead to diabetes later in life.
Original publication:
Belin Selcen Beydag-Tasöz, Joyson Verner D’Costa, Lena Hersemann, Byung Ho Lee, Federica Luppino, Yung Hae Kim, Christoph Zechner, Anne Grapin-Botton. Integrating single-cell imaging and RNA sequencing datasets links differentiation and morphogenetic dynamics of human pancreatic endocrine progenitors. Developmental Cell 2023 Aug 16; doi: 10.1016/j.devcel.2023.07.019
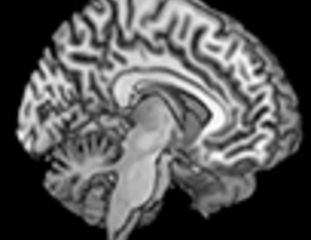
Brain’s Insulin Sensitivity Changes during the Menstrual Cycle
Brain insulin action on peripheral insulin sensitivity in women depends on menstrual cycle phase.
Nature Metabolism 2023
Brain insulin action has an impact on eating behavior, metabolism and body fat distribution – in particular, it increases whole-body insulin sensitivity. However, all of these findings were obtained predominantly in studies involving men. In the journal Nature Metabolism, researchers report that although insulin action in the brain also improves whole-body insulin sensitivity in women, this only occurs during the follicular phase of the menstrual cycle.
Over the last ten years it has been demonstrated that the brain is an insulin-sensitive organ, but also that a substantial number of individuals do not respond to insulin in the brain. This is termed brain insulin resistance. While it is observed especially frequently in people with obesity, genetic factors, elevated blood lipids and impaired insulin transport across the blood-brain barrier also play a role. Preclinical studies also indicate differences between men and women.
Researchers at Ulm University and DZD partners at the Institute for Diabetes Research and Metabolic Diseases (IDM) of Helmholtz Munich at the University of Tübingen and the German Diabetes Center in Dusseldorf studied brain insulin action in 11 women at various stages of the menstrual cycle. The participants were all lean, healthy women with a regular, natural cycle.
Nasal Spray Allows Insulin to Primarily Enter the Brain
Insulin action in the brain was measured using the hyperinsulinemic-euglycemic clamp test after the women had received a nasal spray containing insulin or a placebo. Administered via the nose, substantial amounts of the insulin are delivered into the brain, while only a tiny fraction reaches the bloodstream. Therefore the nasal application allows stimulation of brain insulin action without causing peripheral side effects.
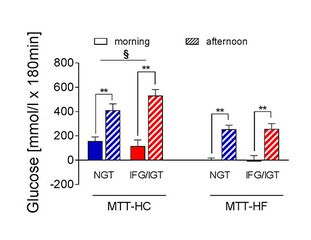
In the follicular phase of the menstrual cycle, the stimulation of the insulin effect in the brain led to an improvement in whole-body insulin sensitivity. In the luteal phase, however, the nasally-administered insulin and the brain insulin action did not have this effect.
Insulin Sensitivity Differs in Follicular and Luteal Phases
The DZD researchers thus found that during the follicular phase of the menstrual cycle there is an increased insulin sensitivity in the brain, which is not seen during the luteal phase.
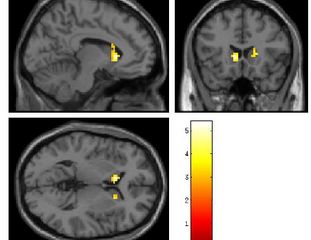
A study of 15 other women, who underwent functional MRT scans on their brains, confirmed these findings. A functional MRT measures insulin sensitivity in the hypothalamus. The change in blood circulation in this brain region is used as a measure of central insulin sensitivity after a nasal administration of insulin. The responsiveness of the hypothalamus was influenced during the follicular phase but not the luteal phase.
The researchers conclude that brain insulin action also improves peripheral insulin sensitivity in women, but only during the follicular phase. They hypothesize that the insulin resistance of the brain in the luteal phase of the menstrual cycle could contribute to whole-body insulin resistance during this time.
Original publication:
Julia Hummel, Charlotte Benkendorff, Louise Fritsche, Katsiaryna Prystupa, Andreas Vosseler, Sofiya Gancheva, Sandra Trenkamp, Andreas L. Birkenfeld, Hubert Preissl, Michael Roden, Hans-Ulrich Häring, Andreas Fritsche, Andreas Peter, Robert Wagner, Stephanie Kullmann, Martin Heni. Brain insulin action on peripheral insulin sensitivity in women depends on menstrual cycle phase. Nat Metab 2023;5:1475–1482; doi:10.1038/s42255-023-00869-w
Understanding Diabetes: Single-Cell Atlas Leverages Machine Learning to Decipher Diabetes at the Molecular Level
Delineating mouse β-cell identity during lifetime and in diabetes with a single cell atlas.
Nature Metabolism 2023
A collaborative endeavor between computer scientists and diabetes researchers at Helmholtz Munich has yielded novel insights into the mechanisms underlying type 1 and type 2 diabetes. This collaboration has resulted in the creation of the first mouse islet atlas (MIA). Leveraging the power of machine learning, the team of scientists integrated single-cell datasets to reveal the molecular alterations that occur during the progression of diabetes and to highlight the distinctions between type 1 and type 2 diabetes. Their findings have been published in 'Nature Metabolism'.
Type 1 (T1D) and type 2 diabetes (T2D) are caused by the loss or dysfunction of the insulin-producing cells in the pancreas, the β-cells, leading to disrupted blood glucose regulation. The β-cells and other cell types in the so-called Langerhans islets of the pancreas communicate with each other and jointly regulate blood glucose levels via hormone secretion. Currently, β-cell function or dysfunction is mainly assessed by measuring the levels of the hormone insulin in the bloodstream. Unfortunately, this is not sufficient to reveal the exact disease-causing mechanism that leads to β-cell failure during autoimmune attack in T1D or are associated with high blood glucose and lipid levels in T2D. Therefore, researchers worldwide studied the gene expression of pancreatic islets in mouse models by analyzing the RNA content within individual cells. This resulted in multiple generated single-cell gene expression (scRNA-seq) datasets. These datasets contain hundreds of thousands of cells with thousands of genes measured in each cell. However, the complexity of these datasets in terms of disease progression, islet cell types, differences in mouse strains and diabetes models as well as laboratory procedures and data processing has hitherto prevented the generation of a consensus on why and how β-cells become dysfunctional during diabetes progression, hindering the understanding of the underlying cause of T1D and T2D.
A team of computer scientists from the research group of Prof. Fabian Theis together with a team led by the diabetes expert Prof. Heiko Lickert, both from Helmholtz Munich, leveraged recent advances in machine learning, particularly deep representation learning and data integration, to develop the mouse islet atlas (MIA). An atlas in the world of cells is a comprehensive collection of data, that provides detailed information about cellular function. These atlases are valuable resources for researchers and scientists studying cellular biology. The MIA integrates nine scRNA-seq datasets and over 300,000 single cells with 1,000-8,000 genes measured per cell. MIA presents the first comprehensive single-cell gene expression resource of mouse pancreatic islets. Through the integration of these big datasets, the scientists were able to decipher how β-cells change their gene expression from healthy to a diseased state in T1D and T2D or in other dysfunction conditions such as aging, enabling the discovery of potential molecular pathways and targets for the prevention of β-cell failure. Furthermore, the integration and direct comparison of data across different datasets and laboratories help to bring consensus into the research community.
Mouse Islet Atlas Deciphers β-Cell Dysfunction
The authors explored the data integrated within MIA, identifying molecular changes shared or specific to T1D and T2D models during disease progression. This revealed that all healthy adult samples contain heterogeneous β-cells, varying in the levels of insulin-production-induced cell stress and aging-associated patterns. MIA also helped to resolve the question of which mouse diabetes models should be used to study human T1D and T2D, thus supporting future experimental study design. The researchers showed that the streptozotocin model, a widely used experimental model of chemical β-cell destruction, which was hitherto used to model both T1D and T2D, better corresponds to T2D when comparing β-cell identities. Additionally, an intermediate β-cell state between healthy and diabetic cells was observed in all diabetes models. This β-cell state and the molecular pathways that are active in these β-cells might be involved in diabetes progression or remission, potentially offering molecular targets for future treatment strategies. Overall, this study is a showcase of how big data integration and the resulting MIA can be exploited to assess a large number of single-cell gene expression datasets generated in many laboratories around the world to find a consensus about diabetes development and new insights that could not have been reached with individual datasets.
The Atlas Represents a Resource for the Future
MIA presents a comprehensive resource, enabling both interactive exploration via cellxgene and computational analysis. For example, MIA can be used to look up which cells express a gene of interest and how strongly the gene is expressed. New samples can be also interpreted in the light of the conditions within MIA by mapping them onto the atlas. In the future, MIA may be further extended and updated to continuously capture newly generated data.
Original publication:
Hrovatin, K. et al. (2023): Delineating mouse β-cell identity during lifetime and in diabetes with a single cell atlas. Nature Metabolism.
Discovery of Possible Biomarker for Prediction of Type 2 Diabetes
Differences in DNA methylation of HAMP in blood cells predicts the development of type 2 diabetes.
Mol Metab 2023
Obesity and non-alcoholic fatty liver disease are two of the main risk factors for type 2 diabetes. If obese individuals develop diabetes, it needs to be detected quickly. Of note, early treatment can prevent diabetic complications. In the journal Molecular Metabolism, researchers report on an epigenetic biomarker that can predict existing type 2 diabetes.
Epigenetic changes enable the DNA to react to environmental influences. A methyl group, linked to a specific DNA sequence, can block or enable the transcription of genes. The epigenetic changes which occur in tissues and or blood cells of a person can determine their eating habits and other aspects of their lifestyle, among other things. Epigenetic factors also play a role in the development of obesity and diabetes.
To find an early and easily-measurable biomarker for the risk of diabetes, researchers at DZD’s partner institution – the German Institute of Human Nutrition (DIfE), Helmholtz Munich, and the associated partner in Lubeck, initially examined the DNA of obese mice.
Comparison of mice with different diabetes risks
Despite their obesity, due to slight differences in their liver fat content, the female mice that were examined had very different diabetes risks: While one group was diabetes-resistant, the other group was especially susceptible to diabetes.
An analysis of gene expression and DNA methylation in the livers of the rodents showed that the HAMP gene expression was reduced by about 50% in diabetes-prone mice in comparison to the diabetes-resistant group. Increased DNA methylation of multiple sites in the gene promoter were found to be the cause for the decreased expression.
HAMP encodes the iron-regulatory hormone hepcidin, which had a lower abundance in the livers of mice prone to developing diabetes.
Confirmation using human test individuals
The researchers also analyzed tissue samples from the livers of obese, insulin-resistant women. They determined that in these individuals, expression of the HAMP gene was significantly downregulated along with increased DNA methylation levels in the promoter at the same sites as the animal model.
However, an easily measurable biomarker should also be easy to access, such as through a blood sample. Therefore, the researchers also analyzed the DNA methylation of the HAMP gene in blood cells, which were taken around four years before the diabetes diagnosis of participants in the prospective EPIC-Potsdam cohort. This also showed a strong association between the methylation at certain CpG sites of the HAMP gene and an increased risk of incident diabetes.
Early marker for existing cases of diabetes
The researchers concluded that their investigations provide new insights into the epigenetic changes of the HAMP gene before the development of type 2 diabetes. The findings also demonstrated that HAMP, or its epigenetic changes, could serve as an early marker for existing type 2 diabetes.
Original publication:
Meriem Ouni, Fabian Eichelmann, Markus Jähnert, Christin Krause, Sophie Saussenthaler, Christiane Ott, Pascal Gottmann, Thilo Speckmann, Peter Huypens, Stefan Wolter, Oliver Mann, Martin Hrabé De Angelis, Johannes Beckers, Henriette Kirchner, Matthias B. Schulze, Annette Schürmann. Differences in DNA methylation of HAMP in blood cells predicts the development of type 2 diabetes. Mol Metab 2023 Sep; doi: 10.1016/j.molmet.2023.101774.
Learning of the Insulin Response
Glucose‑stimulated insulin secretion depends on FFA1 and Gq in neonatal mouse islets.
Diabetologia 2023
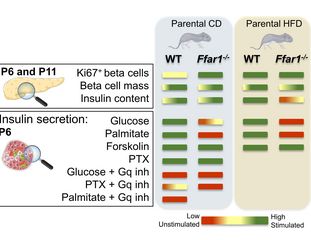
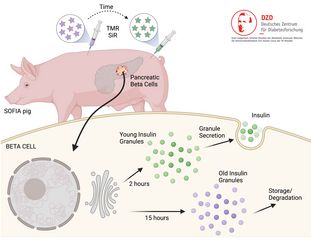
The ability of the pancreatic beta cells to release adequate amounts of insulin to combat increased glucose levels still needs to develop in newborn mice. DZD researchers have discovered that free fatty acid receptor 1 (FFA1) is essential in enabling the progeny to adapt to metabolic challenges, for example, the mother’s high-fat diet. In the future, therapies that target FFA1 may help better protect offspring from the consequences of maternal obesity.
The pancreatic beta cells in newborn mice must undergo various maturation processes before releasing insulin after exposure to glucose. This functional maturation of the beta cells occurs gradually during the early postnatal phase. Environmental factors, such as the mother’s metabolism and breastmilk feeding, play an essential role in the later functionality of the beta cells in the offspring.
FFA1 Enables Adaptation to Metabolic Challenges
Researchers at the DZD partner Institute for Diabetes Research and Metabolic Diseases (IDM) of Helmholtz Munich at the University Hospital Tuebingen investigated the role of free fatty acid receptor 1 (FFA1) in beta cell maturation. The researchers fed wild-type mice possessing intact FFA1 and other animals with an FFA1 knockout mutation either with a high-fat diet or standard diet in the eight weeks before mating and during the gestation and lactation periods.
A High-Fat Diet Causes Increased Blood Sugar Levels in Offspring
At six days old, young mice whose parents possessed the FFA1 knockout mutation and who were given standard feed showed higher blood sugar levels than the offspring of wild-type mice that had also received a regular diet. In contrast, if the parents received a high-fat diet, the wild-type offspring displayed elevated blood sugar levels on day six.
Furthermore, the insulin response of the FFA1 knockout offspring was impaired. Compared to the offspring of the FFA1 knockout mice, the beta cell insulin secretion resulting from increased glucose levels was stimulated four to five times more in the wild-type mice.
A New Target for Protection from Maternal Obesity
The researchers concluded that FFA1 is essential for the development of an adequate insulin response in young mice, enabling them to adjust their insulin secretion to metabolic challenges, such as the high-fat diet of the parents.
In the future, it may be possible to pharmacologically modulate the FFA1 pathways to mitigate the effects of maternal obesity and/or gestational diabetes in the offspring.

© Felicia Gerst (images from bioicons.com)
Original publication:
Lorza‑Gil E, …, Gerst F. Glucose‑stimulated insulin secretion depends on FFA1 and Gq in neonatal mouse islets. Diabetologia, 2023. DOI: 10.1007/s00125-023-05932-5
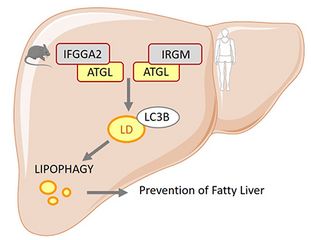
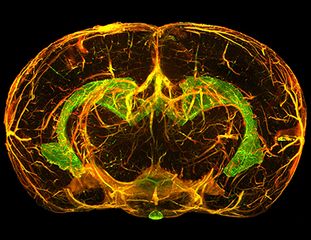
Decoded Mechanism: AgRP Neurons Control Liver Autophagy During Fasting
Nutrient-sensing AgRP neurons relay control of liver autophagy during energy deprivation.
Cell Metab 2023
Autophagy is a crucial metabolic regulator. In a recent study, researchers investigated in-depth how liver autophagy is altered by food deprivation. The AgRP neurons in the hypothalamus, activated by energy deficiency, play a crucial role.
The hypothalamus is essential for energy homeostasis regulation. Special neurons receive hormonal, neuronal, and nutritional physiological signals to fulfill this role. These include AgRP neurons (Agouti-Related Peptide), which recognize and integrate metabolic signals. This helps regulate food ingestion and energy expenditure and maintain glucose homeostasis.
AgRP Neuron-Induced Hepatic Autophagy
A team led by the DZD-associated partner Prof. Jens Brüning from the Max Planck Institute for Metabolism Research in Cologne discovered that fasting in mice activated the AgRP neurons in their hypothalamus. In turn, this induced autophagy in the liver, promoting ketogenesis.
Autophagy is an autonomous cellular process during which digestive components, such as proteins, lipids, and nucleic acids, are transported to the lysosomes. This maintains cellular homeostasis and provides metabolic substrates for energy production during fasting. Further experiments found that AgRP neuron-induced hepatic autophagy depends on neuropeptide Y (NPY) release from the paraventricular nucleus of the hypothalamus (PVH) and activates PVHCRH neurons.
“The activation of the AgRP neurons increased the concentration of circulating corticosteroids,” explains DZD researcher Prof. Dr. Jens Claus Brüning. Hepatic glucocorticoid receptor expression reduction weakened the AgRP neuron-dependent activation of hepatic autophagy. Hepatic autophagy ceased after the researchers inhibited the AgRP neurons during energy deprivation.
Adapting to a Negative Energy Status
The findings indicated the following mechanism: During a short fasting period, AgRP neurons release NPY, promoting a neuronal circuit for PVHCRH activation. This, in turn, activates the hypothalamic-pituitary-adrenal axis and glucocorticoid release, which controls hepatic autophagy.
This enables adaptation to negative energy status. “The results contribute to a better understanding of the regulatory principle of liver autophagy in controlling metabolic adaptation during food deprivation.” says Brüning.
Original publication:
Weiyi Chen, Oliver Mehlkop , Alexandra Scharn, Hendrik Nolte, Paul Klemm, Sinika Henschke, Lukas Steuernagel, Tamara Sotelo-Hitschfeld, Ecem Kaya, Claudia Maria Wunderlich, Thomas Langer, Natalia L Kononenko, Patrick Giavalisco & Jens Claus Brüning. Nutrient-sensing AgRP neurons relay control of liver autophagy during energy deprivation. Cell Metab. 2023 May. doi: 10.1016/j.cmet.2023.03.019.
Colorectal and Pancreatic Cancer: Diabetes Increases the Risk of Cachexia
Diabetes increases mortality in patients with pancreatic and colorectal cancer by promoting cachexia and its associated inflammatory status.
Mol Metab 2023
Patients with colorectal or pancreatic cancer are at increased risk of cachexia if they also suffer from diabetes. They are more likely to experience loss of adipose tissue and skeletal muscles and their symptoms are more pronounced. They also have a lower probability of survival. This was shown in a study published in the specialist journal ‘Molecular Metabolism’ with the participation of the German Center for Diabetes Research (DZD).
Cancer is increasingly being categorized as a complication of diabetes since it is more common in diabetes patients and worsens their prognosis. In turn, cancer patients often develop cachexia. “Cancer-related cachexia could be viewed as a novel complication of diabetes”, says Dr. Alexandra Chovsepian from the Institute for Diabetes and Cancer at Helmholtz Munich, one of the lead authors of the study. “Diabetes should be specifically taken into account during the clinical management of cachexia”.
To determine the extent to which diabetes influences the onset and progression of cachexia, researchers from the DZD and partner institutes conducted a retrospective investigation of a cohort of 345 patients with colorectal or pancreatic cancer.
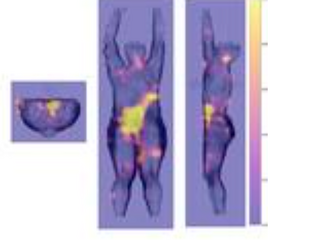
Increased Weight Loss, Lower Probability of Survival
They found there was an increased incidence of cachexia among patients with a history of type 2 diabetes. In total, 80% of them developed cachexia. In contrast, the rate for patients without diabetes was 60%.
Regardless of initial weight and tumor progression, the cancer patients also suffering from diabetes lost more weight than those without diabetes (8.9% vs. 6.0%). In addition, their probability of survival was also lower: 50 per cent of patients without diabetes survived an average of 689 days while those with diabetes survived 538 days.
Patients with pancreatic cancer were especially likely to develop cachexia. A subanalysis of the total cohort showed that diabetes reduced the survival rate and resulted in an even greater weight loss (9.95% vs. 6.93%). Furthermore, the hospitalization duration of these patients was also longer (24.41 vs. 15.85 days).

© Mol Metab / Alexandra Chovsepian (DOI: 10.1016/j.molmet.2023.101729)
Systemic Inflammation May Accelerate Emaciation
There are also differences in the laboratory findings: cancer patients with diabetes had higher C-reactive protein (CRP) and interleukin levels and lower serum albumin levels than patients without diabetes. The changes were particularly notable among cachectic cancer patients with diabetes. Their C-reactive protein levels increased up to 2.300 µg/ml whereas the level for non-diabetic patients was 0.808 μg/ml
“The significant elevation of not only the CRP level but also the other inflammatory markers, such as the platelet to lymphocyte ratio, points to more severe systemic inflammation in patients with diabetes and cachexia”, explains Dr. Olga Prokopchuk from the Clinic and Polyclinic for Surgery at University Hospital rechts der Isar, one of the study’s lead authors. “This may promote systemic metabolic dysfunction and further accelerate cachexia.”
Original publication:
Alexandra Chovsepian, Olga Prokopchuk, Gabriela Petrova, Tefta Gjini, Hanna Kuzi, Simone Heisz, Klaus-Peter Janssen, Marc E. Martignoni, Helmut Friess, Hans Hauner & Maria Rohm. Diabetes increases mortality in patients with pancreatic and colorectal cancer by promoting cachexia and its associated inflammatory status. Mol Metab 2023 Apr 22; doi.org/10.1016/j.molmet.2023.101729
Obesity Surgery Reduces Growth Hormone Levels via Improved Adipose Tissue Function
Metabolic surgery-induced changes of the growth hormone system relate to improved adipose tissue function.
International Journal of Obesity 2023
Weight loss from bariatric surgery can improve not only insulin resistance but also adipose tissue function. Using the metabolic profiles of patients, for the first time, researchers were able to show the correlation between changes in levels of growth hormone and insulin-like growth factor 1 (IGF-1) and improvements in adipose tissue function, although not insulin sensitivity.
In the International Journal of Obesity, researchers from the German Diabetes Center, a DZD partner, published an analysis of 79 obese patients participating in the BARIA-DDZ study. The initial body mass index (BMI) of the patients was 50.8 ± 6.3 kg/m2. They underwent treatment using either sleeve gastrectomy (n=30) or gastric bypass (n=49). Postoperative examinations were carried out at weeks 2, 12, 24, and 52 after surgery. A control group consisting of 24 healthy and lean probands (BMI 24.3 ± 3.1 kg/m2) provided comparative data.
Higher Glycemia and Leptinemia Levels at the Start of the Study
At the start of the study, those who were obese displayed higher blood glucose and leptin levels compared with those of normal weight. Their muscle, adipose tissue, and liver insulin resistance levels were more pronounced than those observed in the control group. Their growth hormone (GH) and IGF binding protein (IGFBP1) levels were lower. In contrast, the IGF-1 levels in both groups were comparable.
At 52 weeks after surgery, patients in the obese groups had lost 33 per cent of their body weight and doubled their muscle insulin sensitivity. This was coupled with a continuous increase in GH, IGF-1 and IGFBP1 and a reduction in leptin levels.
- The GH increase correlated with a reduction in the levels of free fatty acids, adipose tissue insulin resistance, and blood insulin levels, but not with a change in body weight, peripheral insulin sensitivity, or glycemia or leptinemia levels.
- In contrast, the IGF-1 increase correlated with a reduction in the levels of c-reactive protein, a key inflammatory marker.
Summarizing the results, lead author Sofiya Gancheva said that “the changes in GH and IGF-1 following surgically induced weight loss are likely not related to improved leptin secretion or insulin sensitivity, but rather to the restoration of adipose tissue function and improvement of subclinical inflammation”.
Original publication:
Sofiya Gancheva, Sabine Kahl, Christian Herder, Klaus Straßburger, Theresia Sarabhai, Kalliopi Pafili, Julia Szendroedi, Matthias Schlensak & Michael Roden. Metabolic surgery-induced changes of the growth hormone system relate to improved adipose tissue function. International Journal of Obesity 23 Mar 2023, https://doi.org/10.1038/s41366-023-01292-7
Young People with Type 1 Diabetes Experience Fewer Complications when Using a Glucose Sensor
Continuous glucose monitoring versus blood glucose monitoring for risk of severe hypoglycaemia and diabetic ketoacidosis in children, adolescents, and young adults with type 1 diabetes: a population-based study.
The Lancet Diabetes & Endocrinology 2023
Young people with type 1 diabetes who use glucose sensors for continuous glucose monitoring experience fewer acute severe complications. This was shown in a study conducted together with the German Center for Diabetes Research (DZD).
People with diabetes who have well controlled blood sugar levels are less likely to suffer from micro- and macrovascular complications. Although, it is also necessary to prevent acute complications, such as severe hypoglycemia and diabetes ketoacidosis. For young people with type 1 diabetes, it appears that this can be better achieved through continuous glucose monitoring (GCM) via a glucose sensor than conventional blood sugar testing.
In the study, published in Lancet Diabetes & Endocrinology, researchers analyzed the data of more than 32,000 type 1 diabetes patients between the ages of 1.5 and 25 years in Austria, Germany, Luxemburg, and Switzerland. Of these patients, 34% used a glucose sensor for CGM and 66% determined their blood sugar levels themselves using a finger prick test.
“We found that young patients with type 1 diabetes were less likely to develop severe hypoglycemia or diabetic ketoacidosis when using a glucose sensor,” reports Prof. Beate Karges from the Division of Endocrinology and Diabetes at RWTH Aachen University.
Severe Hypoglycemia and Diabetic Ketoacidosis Less Common
Compared to patients using the finger prick test for blood sugar measurement, patients using a glucose sensor were 0.76 times less likely to have severe hypoglycemia and 0.51 times less likely to have diabetic ketoacidosis.
CGM System Provides Data on Risk Parameters
The DZD researchers also investigated whether certain measurement values, provided by the CGM system, were associated with the risk of developing acute complications. They discovered that patients whose glucose levels were below the target value more than 8% of the time were 2.38 times more likely to develop severe hypoglycemia.
Furthermore, when glycemic variability exceeded 36%, severe hypoglycemia was also more common. In contrast, the rate of diabetic ketoacidosis increased when the glucose sensor measured average glucose levels above 180 mg/dl.
CGM Helps Protect Against the Complications of Diabetes
“Our findings show that CGM can help protect young patients with type 1 diabetes from the acute complications of diabetes,” says Karges. “It can also help identify patients who are most at risk of developing such complications, who can then be offered personalized therapy”.
In an editorial, Dr. Alfonso Galderisi and Prof. Jennifer L Sherr, specialists for pediatric endocrinology at Yale University in New Haven, USA, commented that “the findings of this study clearly indicate that this technology helps to reduce the risk of acute diabetic complications”. Through the identification of CGM threshold values, targeted care can be provided to children and adolescents most at risk of developing acute complications.
Original publication:
Karges B, ...., Holl RW. Continuous glucose monitoring versus blood glucose monitoring for risk of severe hypoglycaemia and diabetic ketoacidosis in children, adolescents, and young adults with type 1 diabetes: a population-based study. Lancet Diabetes Endocrinol 2023 Mar 30; https://doi.org/10.1016/S2213-8587(23)00061-X
Editorial:
Galderisi A & Sherr JL. Answering clinically pertinent questions with real-world data from paediatric type 1 diabetes registries. Lancet Diabetes Endocrinol 2023 Mar 30; https://doi.org/10.1016/S2213-8587(23)00085-2
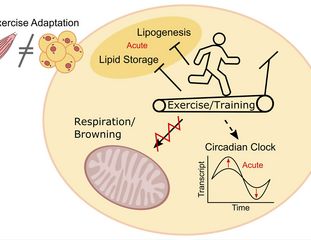
Exercise Promotes Diabetes Prevention in Adipose Tissue
Acute and long-term exercise adaptation of adipose tissue and skeletal muscle in humans: a matched transcriptomics approach after 8-week training-intervention.
International Journal of Obesity 2023
Regular exercise reduces the risk of type 2 diabetes. A study by the German Centre for Diabetes Research (DZD) looked at the role played by the skeletal musculature and the subcutaneous adipose tissue in the health-promoting effects of exercise.
The findings, published in the International Journal of Obesity, show that the subcutaneous adipose tissue also plays a crucial role in the prevention of metabolic diseases, despite it reacting in a very different way to exercise than muscle tissue.
Adjustment at the Molecular Level
“We showed that physical activity leads to molecular level changes in the subcutaneous adipose tissue associated with lipid storage, lipogenesis, and the circadian rhythm. These could combat the progression of metabolic syndrome to type 2 diabetes,” explains DZD researcher Dr. Simon Dreher from Tübingen University Hospital.
“Among other things, regular exercise leads to restoration of a healthy cellular circadian rhythm in obese people,” says Dr Dreher.
The study involved eight women and six men with a predominantly sedentary lifestyle who were either overweight or obese. They completed 8 weeks of supervised endurance training consisting of one hour of training three times per week – 30 minutes cycling and 30 minutes on the treadmill. Samples of subcutaneous adipose tissue and skeletal musculature were taken before and after training for transcriptome analysis.
Exercise Modifies Gene Expression in Fatty Tissue
It was observed that, following the first exercise session, 37 transcripts in the subcutaneous adipose tissue showed acute downregulation or increased regulation. Transcripts of genes associated with lipid metabolism and circadian rhythm were particularly affected.
In contrast, in the muscular tissue, regulation modifications were observed in 394 transcripts after the first exercise session. “There was almost no overlap between fat and muscle tissue, which highlights how differently fat and muscle tissue react to exercise,” says Prof. Cora Weigert, the lead author of the study. “These adjustments in the transcriptome also appear to be long-term as they could also be observed after the 8-week training program”.
An increase in mitochondrial respiration, as observed in the skeletal muscles during physical activity, was not evident in the subcutaneous adipose tissue. Also, no browning of the adipose tissue was observed in the probands.
The changes to the circadian rhythm and lipid metabolism caused by exercise may lead to a healthier metabolism and reduced risk of type 2 diabetes. According to the researchers, understanding how physical activity protects against type 2 diabetes at the molecular level will help create improved diabetes prevention strategies.
Original publication:
Dreher SI, Irmler M, Pivovarova-Ramich O, Kessler K, Jürchott K, Sticht C, Fritsche L, Schneeweiss P, Machann J, Pfeiffer AFH, Hrabě de Angelis M, Beckers J, Birkenfeld AL, Peter A, Niess AM, Weigert C, Moller A. Acute and long-term exercise adaptation of adipose tissue and skeletal muscle in humans: a matched transcriptomics approach after 8-week training-intervention. International Journal of Obesity 2023;47: 313-324; https://doi.org/10.1038/s41366-023-01271-y
Childhood Obesity: Researchers Discover a New Causal Mutation
Aberrant expression of agouti signaling protein (ASIP) as a cause of monogenic severe childhood obesity.
Nature Metabolism 2022
Monogenetic forms of obesity are very rare. Researchers have now discovered a new mechanism linked to severe obesity: overexpression of the ASIP protein. They published details of their findings in Nature Metabolism.
One two-year-old girl was already receiving medical treatment for severe obesity and gigantism. She also showed signs of insulin resistance and hepatic steatosis.
Both parents suffer from obesity. The father has type 2 diabetes, high blood pressure, and gout. The girl shares certain external characteristics (e.g., red hair, pale skin and freckles) with her father. Clinically relevant genetic variants linked to monogenic obesity or other genetic disorders were ruled out via exome sequencing.
However, the phenotype of severe childhood obesity with excessive longitudinal growth, hypopigmentation, and changes to the appetite point to a genetic cause.

© Prof. Antje Körner, University of Leipzig
Molecular Biological Testing of the Stromal Vascular Fraction
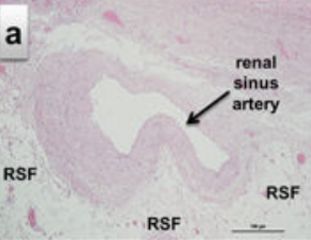
The researchers collected a sample of subcutaneous fatty tissue from the patient during bariatric surgery. They looked for differentially expressed genes in cells of the stromal vascular fraction (SVF) using transcriptome analysis and compared the findings with SVF cells from healthy control subjects. A single gene responsible for Agouti-signaling protein (ASIP) coding showed severe overexpression in the patient’s cells.
The researchers found a heterozygous tandem duplication on the ASIP genomic locus. The mutation places ASIP under the control of a ubiquitously active promoter, causing increased and ubiquitous synthesis of the Agouti-signaling protein, which they were able to demonstrate under experimental conditions.
A Phenotype Observed in Mouse Models
The patient’s phenotype is extremely similar to that seen in the Agouti mouse model. Acting as an antagonist, ASIP suppresses the activation of melanocortin receptors (MCRs), such as MC4R, which can affect eating behavior, energy use, adipocyte differentiation, and pigmentation. The working group confirmed the aberrant ASIP expression in various types of cells from the patient, including induced stem cells, which they were able to differentiate in hypothalamic-like neurons, among others.
Because this mutation is not identified in standard human genetic screening, researchers re-examined the Leipzig Adipose Cohort of 1,745 patients and identified 4 patients with an identical mutation and similar phenotype – a high rate considering the rarity of monogenic obesity.
Thus, for the first time, a genetic form of obesity has been discovered in humans that corresponds to the findings of one of the oldest mouse models. This discovery is not only relevant for the research of pathophysiological correlations and biological feedback loops associated with obesity in humans, but also because genetic diagnostic algorithms will have to be reconsidered, and there may be potential treatment options available for these patients.
Original publication:
Elena Kempf, Kathrin Landgraf, ..., Matthias Blüher & Antje Körner: Aberrant expression of agouti signaling protein (ASIP) as a cause of monogenic severe childhood obesity. Nature Metabolism, 2022. DOI: 10.1038/s42255-022-00703-9
Type 2 Diabetes: Has the Role of Sphingolipids been Deciphered?
Sphingolipid subtypes differentially control proinsulin processing and systemic glucose homeostasis.
Nature Cell Biology 2023
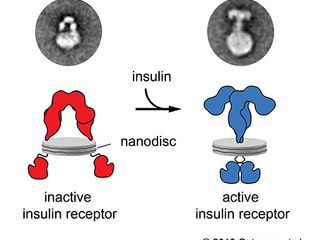
The conversion of proinsulin to insulin in the beta cells of people with diabetes is impaired. In the journal Nature Cell Biology, researchers reported on possible causes: Among others, a loss of function of the CerS2 enzyme, which is responsible for the production of very-long-chain sphingolipids.
Sphingolipid metabolism disorder has previously been linked to obesity. These lipids are essential for almost all types of cells and membranes; however, their role in the beta cells (β cells) has, until now, been unclear.
Under the direction of Dr. Bengt-Frederik Belgardt of the Institute for Vascular and Islet Cell Biology at the German Diabetes Center, researchers in Dusseldorf, Cologne, and Munich, along with researchers from the German Centre for Diabetes Research (DZD), in collaboration with colleagues in Switzerland and Germany, among others, have produced new findings showing that sphingolipids play a crucial role in the processing of proinsulin.
In a type 2 diabetes mouse model, the researchers observed an imbalance affecting certain types of long-chain and very-long-chain sphingolipids in the pancreatic beta cells.
CerS2 Knockout Reduces Insulin Secretion
A potential cause of the observed imbalance is a reduction in ceramide synthase 2 (CerS2) activity. This enzyme is the most common ceramide synthase in human beta cells without diabetes and is necessary for the generation of very-long-chain sphingolipids (also known as VLSLs). If the enzyme stops being produced, this process ceases to function.
CerS2 knockout in the pancreatic beta cells of mice caused reduced insulin content in the beta cells, insulin secretion dysfunction, and glucose tolerance impairment. Furthermore, the reduction of the insulin-to-proinsulin ratio points to limited proinsulin processing.
Proinsulin Processing Depends on Sphingolipids
To gain in-depth insights into the mechanisms, the researchers investigated the various protein interactions. They identified the transport protein Tmed2 as being crucial during proinsulin conversion. Their hypothesis: The binding of sphingolipids with Tmed2 promotes the transport of the Pcsk1 enzyme to the insulin-secreting vesicles.
When the CerS2 enzyme is missing, this affects the binding of sphingolipids to Tmed2, among others, as well as the functioning of the enzyme Pcsk1, which is essential for proinsulin processing. These findings may partially explain the impaired proinsulin to insulin conversion observed in those with type 2 diabetes.
Original publication:
Kerstin Griess, Michael Rieck, Nadine Müller, Gergely Karsai, Sonja Hartwig, Angela Pelligra, Robert Hardt, Caroline Schlegel, Jennifer Kuboth, Celina Uhlemeyer, Sandra Trenkamp, Kay Jeruschke, Jürgen Weiss, Leon Peifer-Weiss, Weiwei Xu, Sandra Cames, Xiaoyan Yi, Miriam Cnop, Mathias Beller, Holger Stark, Arun Kumar Kondadi, Andreas S. Reichert, Daniel Markgraf, Marianne Wammers, Dieter Häussinger, Oliver Kuss, Stefan Lehr, Decio Eizirik, Heiko Lickert, Eckhard Lammert, Michael Roden, Dominic Winter, Hadi Al-Hasani, Doris Höglinger, Thorsten Hornemann, Jens C. Brüning & Bengt-Frederik Belgardt: Sphingolipid subtypes differentially control proinsulin processing and systemic glucose homeostasis. Nature Cell Biology, 2023. DOI: 10.1038/s41556-022-01027-2
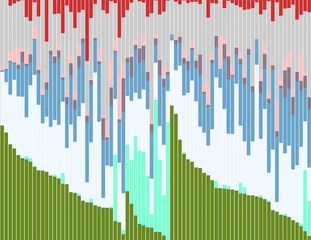
Physical Activity Reduces Risk of Diabetes Complications
Physical Activity and Risk of Major Diabetes-Related Complications in Individuals With Diabetes: A Systematic Review and MetaAnalysis of Observational Studies.
Diabetes Care 2022
Physical activity is a cornerstone in diabetes management; however, evidence synthesis on the association between physical activity and long-term diabetes-related complications is scarce. Researchers from the DZD partner German Diabetes Center have found in a large meta-analysis that exercise is associated with a lower incidence of diabetes-related complications. The results have now been published in Diabetes Care.
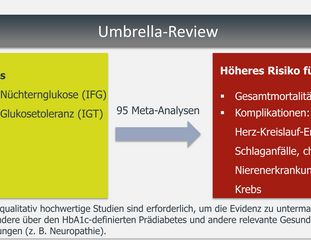
To summarize and evaluate findings on physical activity and diabetes-related complications, the researchers conducted a systematic review and meta-analysis. They included prospective studies investigating the association between physical activity and incidence of and mortality from diabetes-related complications, i.e., cardiovascular disease (CVD), coronary heart disease, cerebrovascular events, heart failure, major adverse cardiovascular events, and microvascular complications such as retinopathy and nephropathy, in individuals with diabetes. Overall, 31 studies published between 1995 and 2021 were included, with examination of populations in the United States, Europe, Asia, and Australia, as well as a cohort from 20 different countries.

Figure: Risk reduction of incidence and mortality of cardiovascular diseases as well as micro-vascular sequelae in persons with diabetes mellitus by physical activity already below WHO recommendation (gray area). Source: Diabetes Care. 2022;45(12):3101-3111. doi:10.2337/dc22-0886
The results of this review, including its meta-analyses, found moderate certainty of evidence that physical activity was associated with reduced relative risk of cardiovascular disease incidence and mortality, as well as overall microvascular complications, particularly retinopathy. The evaluations showed a dose-response relationship, i.e., as physical activity increased, the risk for diabetes sequelae decreased.
Dose-response meta-analyses showed that physical activity was associated with lower risk of diabetes-related complications even at lower levels. These results suggest that even a physical activity level below the WHO recommendation reduces the relative risk for diabetes-related complications.
Original publication:
Rietz M, Schlesinger S et al. Physical Activity and Risk of Major Diabetes-Related Complications in Individuals With Diabetes: A Systematic Review and MetaAnalysis of Observational Studies
Diabetes Care 2022;45(12):3101–3111; https://doi.org/10.2337/dc22-0886
Integrated Treatment of Diabetes and Depression in India is Cost-Effective
Cost-Effectiveness of a Collaborative Care Model Among Patients With Type 2 Diabetes and Depression in India.
Diabetes Care 2022
According to a current study with DZD involvement, integrated treatment of patients with type 2 diabetes and depression in India not only contributes to better patient treatment, but is also more cost-effective. The results are now being published in Diabetes Care.
The researchers analyzed the costs and efficacy across four municipal clinics in India, based on a multi-payer and community perspective. The randomized clinical trial recruited 404 patients with poorly controlled type 2 diabetes (HbA1c ≥8.0%, systolic blood pressure ≥140 mmHg or LDL cholesterol ≥130 mg/dL) and depressive symptoms (9-point Patient Health Questionnaire score of ≥10) who were randomized into two arms: in the first, patients received collaborative care for 12 months, in which they received mental health coaching from non-physician care coordinators, electronic health record management and specialist-supported discussion of their case. This was followed by 12 months of conventional treatment. In the second treatment arm, patients received standard care for 24 months. The study showed that integrated care was not only effective (the clinical results of the INDEPENDENT study were published in the JAMA journal in 2020, https://jamanetwork.com/journals/jama/fullarticle/2769466), but can also be cost-effective. This applies especially if the collaborative care is well integrated into clinical routine and its processes.
The first author Karl Emmert-Fees outlines the results of the study: "The study shows for the first time that integrated care in this type of setting is cost-effective and that its implementation can contribute to better and more efficient care for diabetes and depression in India".
This study can be used to enhance and implement integrated care models for similar contexts and can also contribute to international guidelines on the care of patients with non-communicable diseases and mental health comorbidities.
In the next step, the researchers seek to investigate the long-term effects of the intervention
and identify which components of integrated care have the greatest impact on patient health and the associated costs.
Original publication:
Karl M.F. Emmert-Fees, Michael Laxy, Shivani A. Patel, Kavita Singh, Subramani Poongothai, Viswanathan Mohan, Lydia Chwastiak, K.M. Venkat Narayan, Rajesh Sagar, Aravind R. Sosale, Ranjit Mohan Anjana, Gumpeny R. Sridhar, Nikhil Tandon, Mohammed K. Ali; Cost-Effectiveness of a Collaborative Care Model Among Patients With Type 2 Diabetes and Depression in India. Diabetes Care 2022; dc212533. DOi: https://doi.org/10.2337/dc21-2533
Participants in the study:
Institute of Epidemiology, Helmholtz Munich, Public Health and Prevention, TU Munich, Emory Global Diabetes Research Center, Emory University Atlanta, (USA) Madras Diabetes Research Foundation (Indien)
Type 1 Diabetes: The Increased Prevalence of Metabolic Imbalances in Children during the COVID-19 Pandemic Points to an Unsolved Problem with the Early Diagnosis of Diabetes
Impact of the COVID-19 pandemic on long-term trends in the prevalence of diabetic ketoacidosis at diagnosis of paediatric type 1 diabetes: an international multicentre study based on data from 13 national diabetes registries.
The Lancet Diabetes & Endocrinology 2022
During the COVID-19 pandemic, significantly more children and young people had already developed diabetic ketoacidosis when diagnosed with type 1 diabetes than in previous years. This is the finding of an international multi-center study with DZD participation now published in Lancet Diabetes Endocrinol.
If children and young people have already developed metabolic imbalances (diabetic ketoacidosis) at the time of diagnosis of type 1 diabetes (T1D), this can result in complications such as extended stays in hospital, poorer long-term control of blood sugar levels, brain edema, or even a higher mortality rate. During the COVID-19 pandemic, diabetes centers across the world observed an increased prevalence of diabetic ketoacidosis in diagnosed cases of T1D. DZD researchers, together with international colleagues, investigated whether the number of diabetic ketoacidosis cases associated with the diagnosis of pediatric T1D increased more than expected. To achieve this, they analyzed the number of diabetic ketoacidosis cases before and during the pandemic.
International Multi-center Study
The team evaluated data from 13 national diabetes registers (Australia, Austria, Denmark, Germany, Italy, Luxemburg, New Zealand, Norway, Sweden, Slovenia Czech Republic, USA [Colorado], and Wales). The study cohort consisted of 104,290 children and young people aged between 6 months and 18 years old who were diagnosed with T1D between 1 January 2006 and 31 December 2021. The observed prevalence of diabetic ketoacidosis during 2020 and 2021 was compared with predictions based on the years before the pandemic (2006–2019).
The Increase in the Prevalence of Diabetic Ketoacidosis during the Pandemic was Greater than Expected
Between 2006 and 2019, 23,775 of 87,228 children had diabetic ketoacidosis when diagnosed with T1D (27.3%). The mean annual increase in the prevalence of diabetic ketoacidosis for the entire cohort between 2006 and 2019 was 1.6%. During the pandemic, the numbers were significantly above the predicted prevalences. In 2020, the adjusted observed prevalence of diabetic ketoacidosis was 39.4% (predicted prevalence 32.5%) and 38.9% in 2021 (predicted prevalence 33.0%).
“The increasing prevalence of diabetic ketoacidosis associated with the diagnosis of type 1 diabetes in children is a global problem. There was already an increase in prevalence before the COVID-19 pandemic. During the pandemic, this increase was even greater,” summarizes DZD scientist Prof. Reinhard W. Holl from Ulm University. The authors of the study point out that providing a comprehensive explanation of the classic symptoms of T1D in childhood to the general public, those active in the childcare or daycare settings, and primary care physicians could help raise awareness of the symptoms of T1D. Furthermore, public health measures could be used, e.g., implementing a general islet-cell autoantibodies screening program for children to reduce the number of dangerous metabolic imbalances.
Original publication:
Niels H Birkebaek…Reinhard W Holl, Ondrej Cinek et al.: Impact of the COVID-19 pandemic on long-term trends in the prevalence of diabetic ketoacidosis at diagnosis of paediatric type 1 diabetes: an international multicentre study based on data from 13 national diabetes registries. The Lancet Diabetes & Endocrinology, 2022. DOI: doi.org/10.1016/S2213-8587(22)00246-7.
More Lower Limb Amputations among People with Diabetes in the COVID-19 Pandemic Year 2020
Hospitalisation rate and mortality among people with and without diabetes during the COVID-19 pandemic year 2020.
European Journal of Epidemiology 2022
Fewer people were hospitalized for coronary artery disease, heart attack or diabetic foot syndrome in 2020 than in previous years. However, the number of people with diabetes who were admitted for a lower limb amputation (above the ankle) increased significantly. This is shown by a study by the DZD and DDZ based on data from a German statutory health insurance company. The results of the study have now been published in the European Journal of Epidemiology.
People with diabetes have been seeking medical care less often during the COVID-19 pandemic, which several studies indicate. Reasons for this may be the pandemic-related restrictions of medical services and fear of COVID-19 infection. Researchers from the DDZ and DZD have analyzed the hospitalization and mortality rates of people with and without diabetes in Germany during the COVID-19 pandemic year 2020 compared to 2017-2019. For this purpose, they evaluated the data from a German statutory health insurance company, with which 3.2 million people are insured.
The research team estimated age-sex standardized mortality rates, rates for all-cause hospitalizations, and hospitalization rates due to coronary artery disease, acute myocardial infarction, stroke, diabetic foot syndrome, and above-ankle and below-ankle amputations in people with and without diabetes. Expected rates for 2020 were predicted using Poisson regression based on results from 2017-2019 and compared to observed rates. It was found that the hospitalization rate for lower limb amputations was significantly higher in people with diabetes. However, the hospitalization rate overall and due to coronary heart disease, a heart attack or diabetic foot syndrome was significantly lower. In contrast, mortality and the hospitalization rate for a stroke remained almost unchanged.
The authors of the study emphasize that the increase in hospitalizations due to lower limb amputations in people with diabetes, while the numbers of hospitalizations for diabetic foot syndrome are decreasing, needs special attention.
Original publication:
Narres, M., Claessen, H., Kvitkina, T. … Icks, A. et al.: Hospitalisation rate and mortality among people with and without diabetes during the COVID-19 pandemic year 2020. Eur J Epidemiol 37, 587–590 (2022). doi.org/10.1007/s10654-022-00865-6
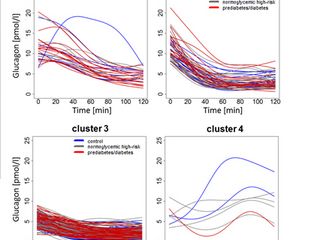
Heterogeneous Development of β-Cell Populations in Diabetes-Resistant and -Susceptible Mice
Heterogeneous Development of β-Cell Populations In Diabetes-Resistant and -Susceptible Mice.
Diabetes 2022
Progressive dysfunction and failure of insulin-releasing β-cells is a hallmark of type 2 diabetes (T2D). DZD researchers have now shown that diabetes resistant and -susceptible mice respond differently to a carbohydrate-rich diet. The gene expression of the beta cells of the diabetes-resistant mice changed in such a way that a protective beta cell cluster developed. In diabetic-prone mice, a failure to adjust gene expression in response to rising blood glucose levels led to increased metabolic stress and beta cell failure. The study was published in the journal Diabetes.
To investigate the mechanisms of beta cell loss in T2D, researchers at the DZD performed single-cell RNA sequencing of islets of Langerhans in two obese mouse strains that differ in their susceptibility to diabetes. Both the diabetes-prone and diabetes-resistant mice have six different groups of beta cells in their islets, which are very similar in abundance before treatment. However, after feeding a carbohydrate-rich diabetogenic diet for two days, the composition of the beta cell clusters differed significantly between the strains. The islet cells of the diabetes-resistant mice developed into a protective beta cell cluster (Beta4). This protective cluster showed indications of reduced beta cell identity (such as downregulation of the GLUT2, GLP1R and MafA genes). Characteristics of mature beta-cell expression decreased. This likely leads to lower glucose uptake and for some, even gain of the ability to divide to ultimately produce more beta cells. An in vitro knockdown of GLUT2 in beta cells led to reduced stress reactions and a decrease in apoptosis markers (apoptosis = programmed cell death). This could explain the improved survival of beta cells in diabetes-resistant mice.
In contrast, beta cells from diabetic-prone mice responded with expression changes indicative of metabolic pressure and stress in the endoplasmic reticulum. They also lacked the adaptation of gene expression towards a more dedifferentiated state. This can presumably contribute to a later loss of beta cells, which in turn contributes to the development of diabetes.
"Our study provides new clues as to why obesity does not always lead to type 2 diabetes. The ability of mice, and presumably humans as well, to respond to elevated blood glucose levels with a transient reduction in their beta cell identity appears to play a key role in protecting them from loss of function and/or apoptosis," said Annette Schürmann, lead author of the study.
About the study:
Researchers from the German Center for Diabetes Research, Helmholtz Munich and the University Hospital Carl Gustav Carus and the Medical Faculty of TU Dresden were involved in the study, which was led by the German Institute of Human Nutrition Potsdam-Rehbruecke (DIfE).
Original publication:
Gottmann P, ..., Schürmann A.: Heterogeneous Development of β-Cell Populations In Diabetes-Resistant and -Susceptible Mice. Diabetes. 2022 Jun 30:db211030. doi: 10.2337/db21-1030. Online ahead of print. PMID: 35771990
Diabetes Subtypes in Children and Adolescents
A classification and regression tree analysis identifies subgroups of childhood type 1 diabetes.
eBioMedicine 2022
An unresolved question has been whether there are different subgroups within young-onset type 1 diabetes. Now a study with DZD participation has identified ten different diabetes subgroups in young people, including seven groups of patients with islet autoantibody-positive type 1 diabetes (autoimmune disease) and three islet autoantibody-negative subgroups. The new findings could enable more precise diabetes prognosis and therapy in the future.
Type 1 diabetes (T1D) is the most common metabolic disease in children and adolescents. Approximately 1.1 million young people worldwide have this autoimmune disease. In T1D, the body produces antibodies against the insulin-producing beta cells (so-called islet autoantibodies) and destroys them. Other forms such as MODY diabetes or type 2 diabetes, in which the hormone insulin is less effective (decreasing insulin sensitivity), are less common in this age group. In order to be able to treat the respective diabetes correctly, an exact diagnosis is necessary. However, the forms of diabetes cannot always be clearly differentiated based on the clinical presentation and the biochemical measurements. The determination of islet autoantibodies and the recording of additional parameters such as beta cell function and insulin sensitivity as well as genetic tests can help distinguish between autoimmune and non-autoimmune forms of diabetes. Thus far it has not yet been clarified whether there are different subtypes in T1D, similar to type 2 diabetes. Studies suggest that there are differences depending on the age at which the disease occurs. For example, genetic load, functional beta cell reserve, and T and B cell responses to autoantigens vary with age at onset of diabetes. In addition, the patients respond differently to therapy depending on their age at the onset of the disease.
The aim of the current study was to use a multivariable approach to identify clinically relevant subgroups of autoimmune and non-autoimmune diabetes. For this purpose, parameters were sought in children and adolescents under 20 years of age with newly diagnosed diabetes that would enable the patients to be grouped with regard to the C-peptide concentration in the blood. The C-peptide is an indicator that insulin is still being formed (residual function of the beta cells).
The researchers identified ten subgroups: seven islet autoantibody-positive (autoimmune disease) and three islet autoantibody-negative. The parameters for the grouping were age, HbA1c value (long-term blood glucose level) and body mass index (BMI). The patients were further characterized based on biochemical measurements. There were significant differences between the groups regarding C-peptide, genetics, inflammatory markers, family history of diabetes, lipids, 25-OH vitamin D3, insulin treatment, insulin sensitivity and insulin autoimmunity. In this way, those examined could be divided into different subgroups with potentially different diabetes developments and prognoses.
In the subgroups of the youngest islet autoantibody-positive children and subjects with the lowest C-peptide levels, inflammatory scores (interferon-ɣ and/or tumor necrosis factor profiles) and insulin autoimmunity were particularly high. The subgroups of older islet autoantibody-positive children and adolescents with higher C-peptide levels showed characteristics that are more indicative of type 2 diabetes (T2D), such as lower insulin sensitivity or high BMI. In the study participants without islet autoantibodies, there were subgroups with values that are more typical of T2D or MODY diabetes, but also those with type 1 diabetes characteristics.
The study included a representative cohort of 1,192 children and adolescents and another independent cohort of 2,722 subjects under 20 years of age with newly diagnosed diabetes. The defined subgroups were found to have prognostic significance. In subjects of the respective subgroups, differences in HbA1c levels were detected even after seven years as shortly after the manifestation of diabetes.
Original publication:
Achenbach et al.: A classification and regression tree analysis identifies subgroups of childhood type 1 diabetes. eBioMedicine, 2022, 82, 104118.
Study on Psychosocial Stress in Type 1 Diabetes
Time With Diabetes Distress and Glycemia-Specific Distress: New Patient-Reported Outcome Measures for the Psychosocial Burden of Diabetes Using Ecological Momentary Assessment in an Observational Study.
Diabetes Care 2022
Many people with diabetes also suffer psychologically from their chronic illness. “Diabetes distress” includes an increased burden of diabetes and depression. In an observational study, DZD researchers have recorded the psychosocial burden of diabetes. The results have appeared in Diabetes Care.
To estimate time with diabetes distress the researcher used ecological momentary assessment (EMA)* in people with type 1 diabetes and analyze its associations with glycemic management based on continuous glucose monitoring (CGM).
The researcher used EMA to assess diabetes distress in a sample of recently hospitalized adults with type 1 diabetes once a day for 17 consecutive days in an ambulatory setting. Additionally, participants were asked daily about hypoglycemia distress (<70 mg/dL [3.9 mmol/L]), hyperglycemia distress (>180 mg/dL [10 mmol/L]), and variability distress (glucose fluctuations). Per person, the percentage of days with elevated distress was calculated (time with distress).
Participants spent a mean (SD) of days in a state of diabetes distress, 54.6 ± 26.0% in hyperglycemia distress, 45.2 ± 27.5% in variability distress, and 23.0 ± 19.3% in hypoglycemia distress.
Time with distress as assessed with EMA showed a comparative advantage over distress as determined by questionnaire-based assessment of diabetes distress regarding associations with glycemic management.
*Ecological momentary assessment (EMA) involves repeated sampling of subjects' current behaviors and experiences in real time, in subjects' natural environments.
Orginal publication:
Ehrmann, D., Schmitt, A. …. Kulzer, B. Hermanns, N. : Time With Diabetes Distress and Glycemia-Specific Distress: New Patient-Reported Outcome Measures for the Psychosocial Burden of Diabetes Using Ecological Momentary Assessment in an Observational Study. Diabetes Care 2022; dc212339. DOI: https://doi.org/10.2337/dc21-2339
A Novel Smartphone App to Change Risk Behaviors of Women after Gestational Diabetes
A novel smartphone app to change risk behaviors of women after gestational diabetes: A randomized controlled trial.
PLoS One 2022
Mothers who had gestational diabetes during pregnancy have an increased risk of developing type 2 diabetes later on. The right lifestyle can significantly reduce this risk. A randomized controlled trial investigated whether the smartphone app TRIANGLE can help with lifestyle changes.
For many young mothers, their own health usually only takes second place after the birth of the child. However, particularly for women who have been diagnosed with gestational diabetes, maintaining a healthy diet, getting sufficient exercise and practicing stress reduction would be important. The right lifestyle can help to reduce the risk of developing type 2 diabetes or cardiovascular diseases later on.
Researchers from the German Center for Diabetes Research (DZD), among others, have developed the smartphone app TRIANGLE to help with lifestyle changes. In a 6-month multicenter, randomized-controlled study, it was investigated whether TRIANGLE helps affected individuals to change their lifestyle compared to standard care.
This first trial did not show the efficacy of the TRIANGLE intervention. However, the app was well accepted and considered helpful by most users. Therefore, this trial supports further development and testing of TRIANGLE and other app interventions for women after GDM. Additionally, it identifies necessary adaptations in trial design to better accommodate non-intensive lifestyle interventions for this target group.
Original publication:
Potzel, A. … Lechner, A.: A novel smartphone app to change risk behaviors of women after gestational diabetes: A randomized controlled trial. PLoS One (April 2022). DOI: doi.org/10.1371/journal.pone.0267258
Covid-19 Increases Risk of Type 2 Diabetes
Incidence of newly diagnosed diabetes after Covid-19.
Diabetologia 2022
People who have had Covid-19 are at increased risk of developing type 2 diabetes. This is the result of a study by DDZ, DZD and IQVIA, which has now been published in ‘Diabetologia’.
Studies show that the human pancreas can also be a target of the SARS-CoV-2 (severe acute respiratory syndrome coronavirus type 2 virus). Following a Covid-19 infection, reduced numbers of insulin secretory granules in beta cells and impaired glucose-stimulated insulin secretion have been observed. In addition, after Covid-19 disease, some patients developed insulin resistance and had elevated blood glucose levels although they had no previous history of diabetes. SARS-CoV-2 infection may lead to a strong release of pro-inflammatory signaling substances (cytokines). Activation of the immune system may persist for months after a SARS-CoV-2 infection and impair insulin effectiveness (muscle, fat cells, liver).
To date, however, it is unclear whether these metabolic changes are transient or whether Covid-19 disease increases the risk of persisting diabetes. To investigate this question, researchers from the German Diabetes Center (DDZ), German Center for Diabetes Research (DZD) and IQVIA (Frankfurt) conducted a retrospective cohort study.
The cohort study included a representative panel of 1,171 physician practices across Germany (March 2020 to January 2021: 8.8 million patients). Follow-up continued until July 2021. "The aim of our study was to investigate the incidence of diabetes after infection with SARS-CoV-2," said first author Wolfgang Rathmann, head of the Epidemiology Research Group at the DDZ. As a control group, the researchers selected people with acute upper respiratory tract infections (AURI), which are also frequently caused by viruses. The two cohorts were matched for sex, age, health insurance, month of Covid-19 or AURI diagnosis, and comorbidities (obesity, hypertension, high cholesterol, heart attack, stroke). Patients on corticosteroid therapy were excluded from the study.
During the study period, 35,865 people were diagnosed with Covid-19. “Our analyses showed that patients with Covid-19 developed type 2 diabetes more frequently than people with AURI. The incidence of diabetes with Covid-19 infection was 15.8 compared to 12.3 per 1000 people per year with AURI. Statistical analysis resulted in an incidence rate ratio (IRR) of 1.28. Put simply, this means that the relative risk of developing type 2 diabetes was 28% higher in the Covid-19 group than in the AURI group,” Rathmann said, summarizing the results.
Although type 2 diabetes is unlikely to be a problem for the vast majority of people with mild Covid-19 disease, the authors recommend that anyone who has recovered from Covid-19 be alert to the warning signs and symptoms, such as fatigue, frequent urination and increased thirst and seek immediate treatment.
Original publication:
Rathmann, W., Kuss, O. & Kostev, K.: .: Incidence of newly diagnosed diabetes after Covid-19. Diabetologia (2022). doi.org/10.1007/s00125-022-05670-0
Prediabetes Can Increase the Risk of Complications
Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies.
Diabetologia 2022
Even the pre-stage to type 2 diabetes increases the risk of serious complications. This was shown in a review by the DZD partner German Diabetes Center.
Prediabetes is a preliminary stage of type 2 diabetes in which glucose metabolism is already disturbed, but glucose or HbA1c levels are not yet high enough to be diagnosed as diabetes. Studies in recent years suggest that even this preliminary stage may be associated with chronic complications and sequelae. In an umbrella review, researchers have compiled a systematic overview of the studies to date and analyzed and evaluated their significance.
To this end, the researchers evaluated 95 meta-analyses. These meta-analyses had included prospective studies of prediabetes and the incidence of diabetes-related complications, comorbidities, or risk of death if they met the following eligibility criteria: Prediabetes had to be defined by blood glucose or HbA1c levels that were above normal but not high enough to be diagnosed as diabetes. Participants had to be adults (≥18 years of age).
The results show that prediabetes is associated with an increased risk of complications such as cardiovascular disease, CHD, stroke, chronic kidney disease, dementia, as well as cancer and higher mortality rates in general. Prediabetes is thus more dangerous than assumed and requires increased attention not only by the scientific community but also in clinical practice. The results are rated as moderately robust, meaning that the findings likely reflect the true association. The certainty of evidence was evaluated by applying the GRADE tool.
The researchers note that further high-quality studies, particularly on HbA1c-defined prediabetes and other relevant health outcomes (e. g. neuropathy) are required to support the evidence.

© DZD
Original publication:
Schlesinger S, Neuenschwander M, Barbaresko J, Lang A, Maalmi H, Rathmann W, Roden M, Herder C. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies. Diabetologia. 2022 Feb;65(2):275-285. doi: 10.1007/s00125-021-05592-3.
Increase in the Incidence of Type 1 Diabetes in Children during the Covid-19 Pandemic
Incidence of Type 1 Diabetes in Children and Adolescents During the COVID-19 Pandemic in Germany: Results From the DPV Registry.
Diabetes Care 2022
During the COVID-19 pandemic, more children and adolescents newly developed type 1 diabetes than in previous years. This is shown by a recent study of the DZD, the University of Giessen and the University of Ulm with co-authors from other centers in Germany, based on the data of the multicenter German Diabetes Prospective Follow-up Registry (DPV*).
The aim of this study was to investigate the incidence of type 1 diabetes in children and adolescents during the COVID-19 pandemic in Germany in comparison to previous years. For this purpose, the researchers recorded the children and adolescents aged between six months and under 18 years newly diagnosed in Germany for the period from January 1, 2020 to June 30, 2021. During this period, 5,162 children and adolescents with new-onset T1D were registered in the DPV. This corresponds to an incidence of 24.4 per 100,000 patient-years. Using Poisson regression models, the researchers determined the expected incidence for 2020/21 from data from 2011 to 2019 to be only 21.2, meaning that the observed incidence during the Corona pandemic was significantly higher than the expected incidence (24.4 [95% CI 23.6-25.2] vs. 21.2 [20.5-21.9]; incidence rate ratios (IRR) 1.15 [1.10-1.20]; P < 0.001).
New cases increased particularly in June 2020 (IRR 1.43 [1.07-1.90]; P 5 0.003), July 2020 (IRR 1.48 [1.12-1.96]; P < 0.001), March 2021 (IRR 1.29 [1.01-1.65]; P 5 0.028), and June 2021 (IRR 1.39 [1.04-1.85]; P 5 0.010). "Type 1 diabetes incidences increased with a delay of about three months after the COVID-19 incidence waves as well as after the pandemic containment measures," reported last author and DZD scientist Prof. Reinhard W. Holl of the University of Ulm. However, the underlying causes for the rise in T1D incidence are still unknown, the researchers emphasize. They consider the increase to be an indirect consequence of the pandemic rather than directly triggered by COVID infection.
* German Diabetes Prospective Follow-up Registry (German abbreviation: DPV):
More than 400 treatment facilities are currently involved in diabetic patient documentation – mainly from Germany and Austria, but also from Luxembourg and Switzerland. The DPV includes data from more than 680,000 patients. The aim of the DPV initiative is to improve treatment outcomes for people with diabetes in routine care through standardized documentation, objective comparison of quality indicators and multicenter therapy research.
Original-Publikation:
Kamrath, C. …. Holl, R. et al.: Incidence of Type 1 Diabetes in Children and Adolescents During the COVID-19 Pandemic in Germany: Results From the DPV Registry. Diabetes Care (2022) DOI: doi.org/10.2337/dc21-0969
Impact of Obesity and Metabolic Disorders on Severity of COVID-19 and Vaccine-Breakthrough Infections
Metabolic disorders, COVID-19 and vaccine-breakthrough infections.
Nature Reviews Endocrinology 2021
Obesity and impaired metabolic health are important risk factors for severe COVID-19. Novel data indicate that these risk factors might also promote vaccine-breakthrough SARS-CoV-2 infections in fully vaccinated people. In a ‘Nature Reviews Endocrinology’ “Year in Review” article DZD-Researcher Norbert Stefan summarizes the most important and up-to-date findings about the relationships of obesity, diabetes and cardiovascular diseases with the severity of COVID-19 and SARS-CoV-2 vaccine-breakthrough infections.
Obesity has now been established as an important determinant of severe COVID-19. Recently published genetic analyses from the large COVID-19 Host Genetics Initiative, applying the Mendelian randomization approach, prove that increased body mass index (BMI) is causally involved in the pathogenesis of the disease.
Novel data from a very large community-based cohort study from the UK that evaluated data from 6,910,695 patients with a positive SARS-CoV-2 test result, found that a high BMI was associated with adverse COVID-19 outcomes, independently of several other COVID-19 risk factors, including type 2 diabetes mellitus (T2DM). A linearly increased risk of hospital admission or death due to COVID-19 was observed at a BMI >23 kg/m2. Importantly, the risk of severe COVID-19 outcomes related to an elevated BMI was highest in the youngest age groups (20–39 years old) and decreased progressively with increasing age.
The author also discusses that accelerated immunosenescence (aging of the immune system) may be an important mechanism explaining the relationship of obesity and T2DM, with severe COVID-19. In this respect he highlights novel data, showing that high glucose levels and insulin resistance, which are frequently found in obesity and T2DM, impair adequate function of CD4+ and CD8+ T cell compartments, resulting in reduced protective antiviral immunity. Furthermore, novel data show that insulin resistance may induce increased infection rates of fat cells and, thereby, progression of COVID-19 in people with SARS-CoV-2 infection.
While vaccination against COVID-19 is highly effective in fighting the COVID-19 pandemic, obesity and/or T2DM may also be involved in immunosenescence related to efficacy of vaccines against SARS-CoV-2. So far, knowledge about this relationship only emerged from few studies. In these studies, among the pre-existing comorbidities, overweight/obesity and T2DM were frequently found in vaccinated patients with severe or critical illness.
Thus, as COVID-19 might become an endemic (regularly found and very common) disease, the role of obesity and impaired metabolic health in promoting SARS-Cov-2 infections and severity of the disease, needs to be taken very seriously. On the other hand, as obesity and impaired metabolic health are modifiable risk factors, there is hope that adequate prevention and treatment of these diseases may be powerful tools to fight the COVID-19 pandemic.
Original-Publikation:
Stefan N.: Metabolic disorders, COVID-19 and vaccine-breakthrough infections. Nat Rev Endocrinol. 2021, https://doi.org/10.1038/s41574-021-00608-9
New Link between Diet, Intestinal Stem Cells and Disease Discovered
Diet-induced alteration of intestinal stem cell function underlies obesity and prediabetes in mice.
Nature Metabolism 2021
Obesity, diabetes and gastrointestinal cancer are frequently linked to an unhealthy diet. However, the molecular mechanisms responsible for this are not fully understood. Researchers at Helmholtz Munich have gained some new insights that help to better understand this connection. These findings provide an important basis for the development of non-invasive therapies.
The intestine is essential for maintaining our energy balance and is a master at reacting quickly to changes in nutrition and nutrient balance. It manages to do this with the help of intestinal cells that among other things are specialized in the absorption of food components or the secretion of hormones. In adult humans, the intestinal cells regenerate every five to seven days. The ability to constantly renew and develop all types of intestinal cells from intestinal stem cells is crucial for the natural adaptability of the digestive system. However, a long-term diet high in sugar and fat disrupts this adaptation and can contribute to the development of obesity, type 2 diabetes and gastrointestinal cancer.
The molecular mechanisms behind this maladaptation are part of the research field of Heiko Lickert and his group at Helmholtz Munich and the Technical University of Munich. The scientists assume that intestinal stem cells play a special role in the maladaptation. Using a mouse model, the researchers investigated the effects of a high-sugar and high-fat diet and compared it with a control group.
From high-calorie diet to increased risk of gastrointestinal cancer
“The first thing we noticed was that the small intestine increases greatly in size on the high-calorie diet,” says study leader Anika Böttcher. “Together with Fabian Theis’ team of computational biologists at Helmholtz Munich, we then profiled 27,000 intestinal cells from control diet and high fat/high sugar diet fed mice. Using new machine learning techniques, we thus found that intestinal stem cells divide and differentiate significantly faster in the mice on an unhealthy diet.” The researchers hypothesize that this is due to an upregulation of the relevant signaling pathways, which is associated with an acceleration of tumour growth in many cancers. “This could be an important link: Diet influences metabolic signaling, which leads to excessive growth of intestinal stem cells and ultimately to an increased risk of gastrointestinal cancer,” says Böttcher.
With the help of this high-resolution technique, the researchers have also been able to study rare cell types in the intestine, for example hormone-secreting cells. Among their findings, they were able to show that an unhealthy diet leads to a reduction in serotonin-producing cells in the intestine. This can result in intestinal inertia (typical of diabetes mellitus) or increased appetite. Furthermore, the study showed that the absorbing cells adapt to the high-fat diet and their functionality increases, thus directly promoting weight gain.
Important basic research for non-invasive therapies
These and other findings from the study lead to a new understanding of disease mechanisms associated with a high-calorie diet. “What we have found out is of crucial importance for developing alternative non-invasive therapies,” says study leader Heiko Lickert, in summarizing the results. To date, there is no pharmacological approach to prevent, stop or reverse obesity and diabetes. Only bariatric surgery causes permanent weight loss and can even lead to remission of diabetes. However, these surgeries are invasive, non-reversible and costly to the healthcare system. Novel non-invasive therapies could happen, for example, at the hormonal level through targeted regulation of serotonin levels. The research group will examine this and other approaches in subsequent studies.
Original publication:
Aliluev et al., 2021: Diet-induced alteration of intestinal stem cell function underlies obesity and prediabetes in mice. Nature Metabolism, DOI: 10.1038/s42255-021-00458-9
Diabetes Diagnosis Based on Whole Body MRI
Diabetes detection from whole-body magnetic resonance imaging using deep learning.
JCI Insight 2021
Type 2 diabetes can be diagnosed with a whole-body magnetic resonance imaging (MRI) scan. This is shown by a current study by researchers from the German Center for Diabetes Research, the Institute of Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen, the Max Planck Institute for Intelligent Systems and Tübingen University Hospital. They used deep learning methods* and data from more than 2000 MRIs to identify patients with (pre-) diabetes. The results have now been published in the journal JCI Insight.
Being overweight and having a lot of body fat increase the risk of diabetes. However, not every overweight person also develops the disease. The decisive factor is where the fat is stored in the body. If fat is stored under the skin, it is less harmful than fat in deeper areas of the abdomen (known as visceral fat). How fat is distributed throughout the body can be easily visualized with whole-body magnetic resonance imaging. "We have now investigated whether type 2 diabetes could also be diagnosed on the basis of certain patterns of body fat distribution using MRI," said last author Prof. Robert Wagner, explaining the researchers' approach.
Deep learning trained with over 2000 MRI scans
To detect such patterns, the researchers used artificial intelligence (AI). They trained deep learning (machine learning) networks with whole-body MRI scans of 2,000 people who had also undergone screening with the oral glucose tolerance test (abbreviated OGTT). The OGTT can screen for impaired glucose metabolism and diagnose diabetes. This is how the AI learned to detect diabetes.
Lower abdominal fat accumulation an important indicator of diabetes pathogenesis
"An analysis of the model results showed that fat accumulation in the lower abdomen plays a crucial role in diabetes detection," Wagner said. Further additional analysis also showed that a proportion of people with prediabetes, as well as people with a diabetes subtype that can lead to kidney disease, can also be identified via MRI scans.
The researchers are now working to decipher the biological regulation of body fat distribution. One goal is to identify the causes of diabetes through new methods such as the use of AI in order to find better preventive and therapeutic options.
*Deep learning is a special method from the field of machine learning with artificial neural networks (ANN) and thus also a sub-area of artificial intelligence (AI). Deep learning is particularly suitable when there is a lot of unstructured data – such as images and scans. In order to teach deep learning algorithms to correctly evaluate images and predict diagnoses, they are trained on annotated (labeled) data.
Original publication
Dietz et al.: Diabetes detection from whole-body magnetic resonance imaging using deep learning. JCI Insight, DOI: doi.org/10.1172/jci.insight.146999
Development of a New in vivo Model for Labeling Secretory Insulin Granule Pools
Sequential in vivo labeling of insulin secretory granule pools in INS-SNAP transgenic pigs.
PNAS 2021
Dysfunction of pancreatic beta cells is a key contributor to type 2 diabetes (T2D). Each beta cell stores insulin in several thousand organelles termed insulin secretory granules (SG), which release insulin extracellularly when blood glucose is elevated. So far, our understanding of the principles governing insulin SG turnover remains very rudimental and derives almost exclusively from ex vivo experiments using isolated pancreatic islets. To overcome the existing translational gap to humans, researchers of the German Center for Diabetes Research (DZD) have developed a new in vivo model (a transgenic pig model) that allows studying secretory insulin granule turnover in vivo.
Pancreatic beta cells produce, store and secrete insulin upon elevated blood glucose levels. However, the highly regulated process of insulin secretion, especially its molecular features and the stimuli behind this process have not yet been fully understood. Furthermore, the current understanding of beta cell function is mostly derived from studies of ex vivo isolated islets in rodent models. To overcome this translational gap and to study insulin secretory granule turnover in vivo, a national research team under the lead of scientists from the DZD-partner Paul Langerhans Institute of the Helmholtz Zentrum München at the University Hospital Carl Gustav Carus and Faculty of Medicine of TU Dresden (PLID) and the LMU Munich has generated a transgenic pig model allowing for the first time the in vivo fluorescent labeling of age-distinct insulin secretory granule pools, hence providing a close-to-life readout of insulin turnover in normoglycemic conditions.
The results of this highly collaborative project have been published in the renowned journal `Proceedings of the National Academy of Sciences of the United States of America (PNAS)`, given the likelihood that this novel large animal model close to humans will provide insight into the turnover of insulin pools in physiological and pathological conditions resembling human type 2 diabetes.
Original publication:
Kemter E., Müller, A., … Wolf, E., Solimena, M.: Sequential in vivo labeling of insulin secretory granule pools in INS-SNAP transgenic pigs. PNAS September 14, 2021 118 (37) e2107665118; https://doi.org/10.1073/pnas.2107665118
In COVID-19 Patients the Virus Also Infects Pancreatic Islet Cells
Viral Infiltration of Pancreatic Islets in Patients with COVID-19.
Nature Communications 2021
In people with COVID-19, the SARS-CoV-2 virus can also infect the pancreatic islet cells and replicate there. This is the result of a recent study in which DZD researchers also participated. The study has now been published in Nature Communications.
Metabolic disorders increase the risk of severe courses of COVID-19 disease. On the other hand, new-onset hyperglycemia (elevated blood glucose levels), metabolic derailments (ketoacidosis), diabetes, and severe metabolic complications of pre-existing diabetes, among others, are also observed in COVID-19 patients. But what is the cause of this? Does the virus also infect the insulin-producing beta cells? Initial studies on stem cells indicated that the SARS-CoV-2 virus can infiltrate and infect human alpha cells and the insulin-producing beta cells of the pancreas and can replicate there. Now, a team of researchers has analyzed pancreatic autopsy tissue from COVID-19 patients. Here, too, they found viral SARS-CoV-2 infiltration of beta cells. Using SARS-CoV-2 pseudoviruses, the team also demonstrated that isolated human islet cells are susceptible (permissive) to infection.
In eleven COVID-19 patients, the team of scientists examined the expression of various receptors and factors that can facilitate viral entry, including ACE2. They found that while 70% of COVID-19 patients expressed ACE2 in the circulatory system, only 30% displayed ACE2 expression in beta cells.
"In summary, using human islet cells and autopsy tissue from patients who died of COVID-19, we have provided unequivocal evidence that beta cells are permissive for infection with SARS-CoV-2," said last author Stefan Bornstein of the DZD-Paul Langerhans Institute Dresden of Helmholtz Zentrum München at the University Hospital and Medical Faculty Carl Gustav Carus of TU Dresden. "However, the exact mechanisms of viral entry are not fully understood at this point, as ACE2 is expressed in beta cells only in a subset of patients."
Original publication:
Steenblock et al.: Viral infiltration of pancreatic islets in patients with COVID-19. Nature Communications (2021) 12:3534, DOI: doi.org/10.1038/s41467-021-23886-3
Development of Novel Blood Glucose-Lowering Dextromethorphan Derivatives That Do Not Affect the Brain
Peripherally Active Dextromethorphan Derivatives Lower Blood Glucose Levels by Targeting Pancreatic Islets.
Cell Chemical Biology 2021
Researchers have chemically modified the active ingredient dextromethorphan (DXM) so that it acts on the pancreatic islet cells and lowers blood glucose levels without affecting the central nervous system. The current results have now been published in Cell Chemical Biology.
The active ingredient dextromethorphan (DXM) is mainly known as a cough suppressant. Studies show that DXM also protects the islet cells of the pancreas and can lower blood glucose levels. However, the drug also affects the brain and can cause dizziness and fatigue. Researchers at the DZD partner German Diabetes Center (DDZ) have now succeeded in chemically modifying DXM in such a way that it no longer passes the blood-brain barrier, but nevertheless fully unfolds its positive effects.
The research team showed that the new DXM derivatives protect murine and human pancreatic islets from cell death. The derivatives also lower blood glucose levels without affecting the behavior of mice. The observation that the new compounds have significantly fewer side effects makes them interesting candidates for future diabetes therapy.
However, the findings may also be interesting for other applications: The active ingredient dextromethorphan is chemically related to morphine. These results show how DXM and possibly other morphinans can be chemically modified so that they have no side effects on the brain and still reach the peripheral tissue.
Original publication:
Scholz, O., Otter, S., Welters, A., Wörmeyer, L., Dolenšek, J., Klemen, S.M., Pohorec, V., Eberhard, D., Mrugala, J., Hamacher, A., Koch, A., Sanz, M., Hoffmann, T., Hogeback, J., Herebian, D., Klöcker, N., Piechot, A., Mayatepek, E., Lammert, E.: Peripherally active dextromethorphan derivatives lower blood glucose levels by targeting pancreatic islets. Cell Chemical Biology. 2021, 11 June, DOI: https://doi.org/10.1016/j.chembiol.2021.05.011
New Mechanism Discovered: How Higher Leptin Levels Can Lead to Hypertension
Obesity-Associated Hyperleptinemia Alters the Gliovascular Interface of the Hypothalamus to Promote Hypertension.
Nature Metabolism 2021
Researchers have shown for the first time the role of astrocytes in the hypothalamus in obesity-related hypertension and how the hormone leptin is involved in the increase of blood vessels in the hypothalamus of obese mice. The study was published in Nature Metabolism.
Pathologies of the micro- and macrovascular systems are a hallmark of the metabolic syndrome, which can lead to chronically elevated blood pressure. However, the underlying pathomechanisms involved still need to be clarified. Researchers have now shown for the first time that an obesity-associated increases in serum leptin triggers the select expansion of the micro-angioarchitecture in pre-autonomic brain centers that regulate hemodynamic homeostasis.
Once the researchers increased the hormone leptin in these mice, certain brain cells, the astrocytes, boosted the production of a specific growth factor. This growth factor, in turn, promoted vessel growth. The result was an increased number of vessels in the hypothalamus (and no other brain region).
When the researchers increased leptin levels, certain brain cells, astrocytes, boosted the production of a specific growth factor. This growth factor, in turn, promoted vessel growth. The result was an increased number of vessels in the hypothalamus (and no other brain region). The scientists thus demonstrated that leptin is mainly responsible for the increased concentration of vessels in the hypothalamus and that this process is mediated via astrocytes.
The study was led by Helmholtz Zentrum München, and researchers from Ludwig-Maximilians-Universität, Technische Universität München and the German Diabetes Center were also involved.
Original publication:
Gruber et al., 2021: Obesity-associated hyperleptinemia alters the gliovascular interface of the hypothalamus to promote hypertension. Nature Metabolism, DOI: 10.1016/j.cmet.2021.04.007
Highlight-Artikel in Nature Reviews Endocrinology: https://www.nature.com/articles/s41574-021-00511-3
A High BMI Has a Negative Effect on Socioeconomic Status
The Effect of BMI and Type 2 Diabetes on Socioeconomic Status: A Two-Sample Multivariable Mendelian Randomization Study.
Diabetes Care 2021
People with a high body mass index (BMI) often have a low income and live in areas with higher regional deprivation*. Researchers at Helmholtz Zentrum München and the German Center for Diabetes Research (DZD) have shown in a study that there is a causal relationship between high BMI and low socioeconomic status. The study was published in Diabetes Care and was conducted in cooperation with researchers from LMU (Munich School of Management and Munich Center of Health Sciences) and TUM (Public Health and Prevention).
Previous evidence indicates that people with severe overweight and type 2 diabetes (T2D) also have poorer labor market prospects and a lower income. In the present study, researchers have now investigated the causal effect of a high BMI and T2D on socioeconomic status using a special study design (Mendelian randomization). The genetic influence – that is, independent of environmental influences – of BMI and diabetes were taken into account.
People with a higher BMI were found to be more likely to have low incomes and to live in areas of higher deprivation. Reasons for this may include lower ability to work, higher absenteeism, higher likelihood of musculoskeletal disorders or higher social discrimination. These factors may in turn lead to poorer career prospects, decreasing labor market participation and lower income, the authors conclude. Lower income could in turn lead to people moving to disadvantaged areas with more affordable housing and food options.
However, the studies did not show any negative influence of type 2 diabetes on socioeconomic status. The authors encourage further research to investigate in more detail the effects of T2D on socio-economic status using new genome-wide association studies. In addition, the mechanisms that lead to a disadvantage for people with an increased BMI should be further investigated.
Original publication:
Sara Pedron et al: The Effect of BMI and Type 2 Diabetes on Socioeconomic Status: A Two-Sample Multivariable Mendelian Randomization Study. Diabetes Care 2021 Mar; 44(3): 850-852. DOI: https://doi.org/10.2337/dc20-1721
* Regional deprivation
Regional deprivation is a measure of social inequality and describes material differences between regions or areas based on variables such as the unemployment rate, ownership of a house or car, and living space per household member.
Risk of Type 1 Diabetes Declines With Age
An Age-Related Exponential Decline in the Risk of Multiple Islet Autoantibody Seroconversion During Childhood.
Diabetes Care, 2021
The risk of developing islet autoimmunity and type 1 diabetes declines exponentially with age. This is the result of a recent analysis of the TEDDY study, which has now been published in Diabetes Care. The new findings may also improve screening for pre-symptomatic type 1 diabetes.
Islet autoimmunity develops before clinical type 1 (T1D) diabetes and includes multiple and single autoantibody phenotypes. The objective was to determine age-related risks of islet autoantibodies that reflect etiology and improve screening for pre-symptomatic T1D. For this purpose, the researchers prospectively monitored 8,556 genetically at-risk children at 3- to 6-month intervals from birth for the development of islet autoantibodies and T1D.
The results showed that the 5-year risk of developing multiple islet autoantibodies was 4.3 per cent at 7.5 months of age. At an age of just over six years, it declined to 1.1 percent. The authors of the study therefore suspect that the risk of developing islet autoimmunity declines exponentially with age and the influence of major genetic factors on this risk is limited to the first few years of life.
The new findings may also help to improve screening for pre-symptomatic T1D. The study showed that testing twice for islet autoantibodies, first at two years of age and then again at 5-7 years of age, had the highest sensitivity and positive predictive value of multiple islet autoantibody phenotypes for T1D.
According to the authors, one strength of the current evaluation is the large number of robust data collected in the TEDDY study. One limitation is that all TEDDY children have a certain genetic constellation, which was determined as an inclusion criterion for the TEDDY study. Thus, the study population does not quite correspond to the general population.
Original publication:
Bonifacio, E. et al.: An age-related exponential decline in the risk of multiple islet autoantibody seroconversion during childhood. DOI: https://doi.org/10.2337/dc20-2122
*About the TEDDY study
The TEDDY study (The Environmental Determinants of Diabetes in the Young), is an international research project (USA, Finland, Germany and Sweden) that investigates the possible risk factors for the development of type 1 diabetes. More than 8,600 newborns with an increased genetic risk for T1D were included in the study and closely monitored until their teenage years. The vast majority of the participating children (89 percent) had no close relatives with type 1 diabetes.
https://teddy.epi.usf.edu
The Longevity Gene mINDY (I’m Not Dead, Yet) not only Prevents Metabolic Disease, but also Lowers Arterial Blood Pressure and Heart Rate
The Longevity Gene mINDY (I’m Not Dead, Yet) Affects Blood Pressure Through Sympathoadrenal Mechanisms.
JCI Insight, 2021
Authors from the German Center for Diabetes Research (DZD) presented data showing that the longevity gene mammalian Indy (mINDY) is involved in blood pressure regulation in the Journal of Clinical Investigation (JCI) insight. Reduced expression of mINDY, which is known to extend life span in lower organisms and to prevent from diet induced obesity, fatty liver and insulin resistance in mice, has now been shown to lower blood pressure and heart rate in rodents. The authors provided mechanistic insights for the underlying physiological mechanism based on in vivo data in a genetic knock out model as well as microarray and in vitro studies. Furthermore, the hypothesis is supported by confirming critical effects in vitro using a small molecule inhibitor of mINDY. The authors conclude that deletion of mIndy recapitulates beneficial cardiovascular and metabolic responses to caloric restriction, making it an attractive therapeutic target.
Andreas Birkenfeld and colleagues provide a comprehensive study showing that mIndy deletion attenuates sympathoadrenal support of blood pressure and reduced arterial blood pressure and heart rate in a muine knockout model. Blood pressure was assessed invasively using intra-arterial pressure probes over several days. Urinary analysis for catecholamines and metanephrines as well as unbiased transcriptomic analysis of adrenal glands identified the affected biosynthetic pathways. Indeed, catecholamine biosynthesis was attenuated in mINDY-KO adrenals, whereas plasma steroids and steroid hormone synthesis were unaffected.
In vitro studies on an adrenal cell line supported this hypothesis. mIndy codes for a is a carboxylic acid transporter protein expressed in plasma membrane. Citrate, the main substrate of the mINDY transporter, increased catecholamine content, while pharmacological inhibition of mINDY by a small molecule inhibitor blunted the effect.
The study provided further insights into the physiological mechanisms of the beneficial effects of reducing mINDY activity which is known to protect from diet and aging induced metabolic diseases by mechanisms akin to caloric restriction. Therefore, the data showed a novel mechanism contributing to a cardiometabolic cross talk and further supporting mINDY as a promising target for the whole spectrum of metabolic syndrome components, including increased blood pressure.
The study was published from the Institute of Diabetes Research and Metabolic Disorders (IDM) of the Helmholtz Center Munich at the University Tübingen and the Clinic of Diabetes, Endocrinology and Nephrology of the University Hospital Tübingen.
Original publication:
Willmes DM et al.: The longevity gene mIndy (I’m Not Dead, Yet) affects blood pressure through sympathoadrenal mechanisms. JCI Insight. 2021, https://doi.org/10.1172/jci.insight.136083.
Use of Diabetes Technologies also Depends on Socio-Economic Status
A Decade of Disparities in Diabetes Technology Use and HbA 1c in Pediatric Type 1 Diabetes: A Transatlantic Comparison.
Diabetes Care, 2020
Insulin pumps, continuous glucose monitors (CGMs) - over the past decade, the use of diabetes technologies to manage type 1 diabetes in children and adolescents has increased worldwide. Researchers at the DZD in Düsseldorf, Munich and Ulm, together with colleagues from the USA, have investigated whether inequality in access to these technologies based on socioeconomic status (SES) also leads to different levels of blood glucose (HbA1c). Their study, now published in Diabetes Care, shows " A decade of disparities in diabetes technology use and HbA1c in pediatric type 1 diabetes: A transatlantic Comparison".
For the study, researchers examined the use of diabetes technology and HbA1c levels in children and adolescents under 18 years of age from the Type 1 Diabetes Exchange (T1DX, USA, n = 16,457) and Diabetes Prospective Follow-up (DPV, Germany, n = 39,836) registries by socioeconomic status (SES) between two time periods 2010-2012 and 2016-2018. For this purpose, the registers were divided into quintiles. For categorisation into Q1 (lowest SES) to Q5 (highest SES), insurance type, education level and annual income, among others, were used.
The study showed that participants with lower SES had higher HbA1c (in 2010-2012 and 2016-2018, respectively: 8.0% and 7.8% in Q1 and 7.6% and 7.5% in Q5 for DPV; 9.0% and 9.3% in Q1 and 7.8% and 8.0% in Q5 for T1DX). For DPV, the association between SES and HbA1c did not change between the two time periods, whereas for T1DX, disparities in HbA1c by SES increased significantly (P < 0.001). After adjusting for technology use, results for DPV did not change, whereas the increase in T1DX was no longer significant.
Although no causal conclusions can be drawn, diabetes technology use is lowest and HbA1c is highest in those of the lowest SES quintile in the T1DX, and this difference for HbA1c broadened in the past decade. Associations of SES with technology use and HbA1c were weaker in the DPV registry.
Original publication:
Addala et al.: A Decade of Disparities in Diabetes Technology Use and HbA 1c in Pediatric Type 1 Diabetes: A Transatlantic Comparison. Diabetes Care (2020); DOI: 10.2337/dc20-0257
High Resolution 3D Microscopy Enables to Reconstruct the Highways of Insulin Transport
Three-Dimensional Fib-Sem Reconstruction of Microtubule-Organelle Interaction in Whole Primary Mouse Beta Cells.
Journal of Cell Biology, 2020
Microtubules are a part of cytoskeleton and act as highways for the transport of vesicles within the cell. However, their role in insulin transport and secretion is currently under debate. Now, an international team led by scientists of the Paul-Langerhans-Institute Dresden, a partner of the German Center of Diabetes Research (DZD), together with the CSBD, MPI-CBG, Janelia Research Campus, CMCB, Fondazione Human Technopole as well as the EPFL used high resolution 3D electron microscopy to image insulin secreting pancreatic islet beta cells in their entirety at an unprecedented resolution and reconstructed all insulin secretory granules, microtubules, mitochondria, Golgi apparati, and centrioles to generate a comprehensive spatial map of microtubule-organelle interactions. The outcome of this highly collaborative project was now published in the renowned journal “Journal of Cell Biology”.
Links:
Segmentation masks and crops of analyzed beta cells
Full resolution beta cell volume for browsing
Original publication:
Müller A, Schmidt D, Shan Xu C, Pang S, Verner D’Costa J, Kretschmar S, Münster C, Kurth T, Jug F, Weigert M, Hess HF, Solimena M., Three-dimensional Fib-Sem reconstruction of microtubule-organelle interaction in whole primary mouse beta cells. Journal of Cell Biology (2020), DOI: https://doi.org/10.1083/jcb.202010039
Pancreatic Steatosis Associates With Impaired Insulin Secretion
Pancreatic Steatosis Associates With Impaired Insulin Secretion in Genetically Predisposed Individuals.
The Journal of Clinical Endocrinology & Metabolism, 2020
In people with a high genetic risk for diabetes, a pancreatic steatosis can lead to a decrease in insulin secretion. This is indicated by studies of the DZD, which have now been published in The Journal of Clinical Endocrinology & Metabolism.
So far, there are conflicting evidence on whether and how pancreatic steatosis affects insulin secretion. Accumulating evidence implicates that fat compartment as a modulator of islet function. Specifically, pancreatic steatosis was inversely associated with insulin secretion in subjects with prediabetes. However, subjects with normal glucose tolerance do not exhibit the negative association between pancreatic steatosis and insulin secretion. Researchers at the DZD in Tübingen therefore suspect that pancreatic steatosis only has a negative effect on the function of beta cells if there is a genetic predisposition for diabetes.
To test this hypothesis, they investigated the interaction between genotype and fat in the pancreas on insulin secretion. To this end, they evaluated the data of 360 nondiabetic individuals with elevated risk for T2D from the Tuebingen Family Study (TUEF), and 64 patients undergoing pancreatectomy. The fat content of the pancreas was measured by magnetic resonance imaging (MRI) and the genetic risk score for type 2 diabetes was determined. Insulin secretion was determined by oral glucose tolerance testing and fasting blood sampling prior to surgery.
There was a negative association between pancreatic fat and insulin secretion in participants with high genetic risk. However, individuals with low genetic risk showed a positive correlation between pancreatic fat and insulin secretion. The researchers suspect that only genetic insulin resistance leads to pancreatic fat becoming harmful to insulin secretion.
Original publication:
Róbert Wagner et al: Pancreatic Steatosis Associates With Impaired Insulin Secretion in Genetically Predisposed Individuals. The Journal of Clinical Endocrinology & Metabolism, Volume 105, Issue 11, November 2020, dgaa435, https://doi.org/10.1210/clinem/dgaa435
Different Response of Mitochondrial Respiration in Skeletal Muscle and Adipose Tissue to Endurance Exercise
Response of mitochondrial respiration in adipose tissue and muscle to 8 weeks of endurance exercise in obese subjects.
The Journal of Clinical Endocrinology & Metabolism, 2020
In obese individuals, endurance exercise improves fitness and increases the number of mitochondria * and cellular respiration in skeletal muscles. However, the intervention has no effect on cellular respiration in adipose tissue. This is the result of a study by DZD researchers that has now been published in The Journal of Clinical Endocrinology & Metabolism.
Studies in rodents suggest that exercise not only increases the number of mitochondria and the respiratory capacity of skeletal muscles, but also in adipose tissue. In a study, researchers at the DZD in Tübingen investigated the effects of endurance training on cellular respiration in the human skeletal muscles and abdominal adipose tissue and whether there is a direct connection between increased cellular respiration and improved insulin sensitivity. For this purpose, the researchers carried out an 8-week aerobic endurance training intervention with 25 untrained test subjects (16 women, 9 men aged 29.8 ± 8.4 years) who were overweight or obese. The researchers then analyzed mitochondrial respiration in skeletal muscle fibers and in the subcutaneous adipose tissue of the abdomen.
Based on the change in insulin sensitivity after the intervention, the subjects were grouped into responders (subjects whose insulin sensitivity increased) and low responders (subjects whose insulin sensitivity did not increase significantly). In both groups, fitness, cellular respiration and the amount of mitochondrial enzymes in the skeletal muscles improved equally. The endurance training had no effect on the mitochondria in the abdominal subcutaneous adipose tissue. Another interesting finding of the study is that women exhibited higher cellular respiration in adipose tissue than men.
“Our data show that the increase in the mitochondrial respiratory capacity of the skeletal muscles after endurance training has no predictive power for the improvement of the peripheral insulin sensitivity. Furthermore, the endurance training does not increase cellular respiration in the subcutaneous adipose tissue, with a simultaneous decrease in this fat compartment,“ said Cora Weigert of the DZD partner Institute for Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen, summarizing the findings.
* Mitochondria are the "power plants" of the cells and play a central role in cellular energy production. In a process known as cellular respiration, glucose and fatty acids are converted with oxygen into carbon dioxide and water, creating adenosine triphosphate (ATP), the energy carrier of the cells.
Original publication:
Hoffmann, C. et al.: Response of mitochondrial respiration in adipose tissue and muscle to 8 weeks of endurance exercise in obese subjects. The Journal of Clinical Endocrinology & Metabolism (2020) DOI: 10.1210/clinem/dgaa571
High Protein Diet Reduces Liver Fat
High-protein diet more effectively reduces hepaticfat than low-protein diet despite lower autophagy and FGF21 levels.
Liver International, 2020
Non-alcoholic fatty liver diseases (NAFLD) are particularly widespread in industrialized countries. Lifestyle changes with a balanced diet and increased exercise are still the treatment of choice for fatty liver disease. DZD researchers were able to show that a calorie-reduced diet with a high protein content reduced liver fat more effectively than a calorie-reduced low-protein diet. The results were published in the journal Liver International.
The researchers investigated how the protein content of the diet affects the amount of liver fat in severely overweight people with a non-alcoholic fatty liver. For this purpose, 19 participants with morbid obesity undergoing bariatric surgery were randomized into two hypocaloric (1500‐1600 kcal/day) diet groups, a low protein (LP) and a high protein (HP), for three weeks prior to surgery. Intrahepatic lipid levels (IHL) and serum fibroblast growth factor 21 (FGF21) were measured before and after the dietary intervention. Autophagy flux, histology, mitochondrial activity and gene expression analyses were performed in liver samples collected during surgery.
The group that received a high-protein diet lost about five kilograms and IHL levels decreased by 42.6 %. In the LP group, IHL values did not change significantly despite similar weight loss. Hepatic autophagy flux and serum FGF21 increased by 66.7% and 42.2%, respectively, after 3 weeks in the LP group only. Expression levels of fat uptake and lipid biosynthesis genes were lower in the HP group compared with those in the LP group. RNA‐seq analysis revealed lower activity of inflammatory pathways upon HP diet. Hepatic mitochondrial activity and expression of β‐oxidation genes did not increase in the HP group.
The HP diet reduces liver fat more effectively than the LP diet despite less autophagy. The data suggest that the liver fat reduction in HP diet results primarily from the suppression of fat absorption and lipid biosynthesis.
Original publication:
Xu, C., Markova, M., Seebeck, N., Loft, A., Hornemann, S., Gantert, T., Kabisch, S., Herz, K., Loske, J., Ost, M., Coleman, V., Klauschen, F., Rosenthal, A., Lange, V., Machann, J., Klaus, S., Grune, T., Herzig, S., Pivovarova-Ramich, O., Pfeiffer, A. F. H.: High-protein diet more effectively reduces hepaticfat than low-protein diet despite lower autophagy and FGF21 levels. Liver Inter. in press (E-pub ahead of print) (2020). [Open Access] [https://doi.org/10.1111/liv.14596]
How Insulin in the Brain Controls Metabolism and Food Intake
Central nervous pathways of insulin action in the control of metabolism and food intake.
The Lancet Diabetes & Endocrinology, 2020
The brain is an insulin-sensitive organ. A number of areas of the brain react to insulin, such as areas that are important for food intake, metabolism and memory. In a review article in The Lancet Diabetes & Endocrinology, DZD researchers provide an overview of recent studies investigating how insulin acts on the CNS to modulate behaviour and systemic metabolism. Disturbances in brain insulin action represent a possible link between metabolic and cognitive health.
Current findings from human research suggest that boosting central insulin action in the brain modulates peripheral metabolism, enhancing whole-body insulin sensitivity and suppressing endogenous glucose production. Moreover, central insulin action curbs food intake by reducing the salience of highly palatable food cues and increasing cognitive control.
Research in rodents and humans shows that the mesocorticolimbic circuitry is finely tuned in response to insulin, driven mainly by the dopamine system. These mechanisms are impaired in people with obesity, which might increase their risk of developing type 2 diabetes and associated diseases. Overall, current findings highlight the role of insulin action in the brain and its consequences on peripheral metabolism and cognition.
Original publication:
Kullmann et al: Central nervous pathways of insulin action in the control of metabolism and food intake. The Lancet Diabetes & Endocrinology (2020), DOI: https://doi.org/10.1016/S2213-8587(20)30113-3
Additional Genetic Cause for NAFLD Discovered
Immunity-related GTPase induces lipophagy to prevent excess hepatic lipid accumulation.
Journal of Hepatology, 2020
The cause of non-alcoholic fatty liver disease (NAFLD) is multifactorial, including genetic and environmental factors. Currently, only a few genetic variants explain the heritability of the disease. DZD researchers have now discovered new genes that play a role in the development of fatty liver. The results have been published in the Journal of Hepatology.
Non-alcoholic fatty liver disease (NAFLD) is the leading cause of chronic liver disease in Europe and the United States. In addition to an unhealthy lifestyle with a high-fat, high-sugar diet and lack of exercise, a genetic predisposition is also responsible for the development of this liver disease.
Using molecular markers and statistical methods – quantitative trait locus (QTL) analysis – genes that cause complex human diseases can be identified in mouse strains. Researchers have now discovered a new family of genes that play an important role in preventing fatty liver development. In humans and mice, the genes IRGM, Ifgga2 and Ifgga4 produce regulatory proteins from the family of immunity-related GTPases that counteract fat accumulation in the liver. However, if there is a genetic modification, fewer proteins are formed. Studies show that the liver of patients with NAFLD and mice with fatty liver have significantly lower amounts of these proteins.
Functional studies have shown that an overproduction of immunity-related GTPases in liver cells or in the liver of mice, significantly reduced their fat content. The reason for this is the induction of a particular form of autophagy that is specific for the degradation of fats and is therefore called lipophagy.
“Our work has identified further important genes that cause fatty liver disease. The study results also deepen our understanding of which cellular processes have to be stimulated to counteract fatty liver development,” said Professor Annette Schürmann, head of the Department of Experimental Diabetology at the German Institute of Human Nutrition Potsdam-Rehbrücke (DIfE) and spokesperson for the German Center for Diabetes Research (DZD).
Original publication:
Schwerbel, K. et al: Immunity-related GTPase induces lipophagy to prevent excess hepatic lipid accumulation. Journal of Hepatology (2020); DOI: https://doi.org/10.1016/j.jhep.2020.04.031
Beta Cell Dysfunction Is a Hallmark of Early Type 2 Diabetes Pathogenesis
Dysfunction of Persisting β-Cells is a Key Feature of Early Type 2 Diabetes Pathogenesis.
Cell Reports, 2020
Already at an early stage of type 2 diabetes pathogenesis, the function of the insulin-producing beta cells deteriorates. The number of beta cells is unchanged at this stage. This is the result of a study recently published in Cell Reports by scientists of the German Center for Diabetes Research.
Type 2 diabetes is not only characterized by insulin resistance, but also by the fact that the pancreas produces less insulin. However, it has so far been unclear whether the insufficient insulin level during the development of the disease can be attributed to a dysfunction of the beta cells or to the loss of the beta cell mass. In order to gain new insights here, researchers led by Professor Stephan Speier have used a novel in situ platform for investigating the human pancreas in diabetes pathogenesis. Researchers from the DZD, the Paul Langerhans Institute in Dresden of Helmholtz Zentrum München and the Faculty of Medicine Carl Gustav Carus of TU Dresden, University Hospital Dresden and King's College London were involved in the study.
The group used freshly resected living pancreatic tissue to analyze the function of the beta cells in their original organ environment and to determine the beta cell volume. The tissues examined in this study came from donors from a larger patient cohort who had been metabolically phenotyped prior to pancreatectomy. The group included people without diabetes (ND), people with restricted glucose tolerance (IGT) and people with type 2 diabetes and thus represented the entire development spectrum of T2D pathogenesis. "After the production of 120 µm thick tissue sections, we were able to quantify glucose-induced insulin secretion in the tissue of test subjects under almost physiological conditions and, in parallel, examine the 3D cell morphology on adjacent sections," said the first author, Dr. Christian Cohrs from PLID and the DZD. This novel in situ approach for human pancreatic tissue sections made it possible for the first time to simultaneously investigate beta cell mass and function and to correlate these with the patients' diabetes status.
"Our data demonstrate that beta cells exhibit significant functional deterioration and exhaustion in early stages of T2D pathogenesis, when subjects have impaired glucose tolerance but are not yet diabetic. In contrast, beta cell numbers in the investigated tissues are maintained at this stage of the disease process," said Professor Speier, research group leader at the Paul Langerhans Institute Dresden (PLID) and professor at the Institute of Physiology of TU Dresden. "Thus, our results identify beta cell dysfunction as an initial feature of diabetes development.”
Original publication:
Cohrs CM, Panzer JK, Drotar DM, Enos SJ, Kipke N, Chen C, Bozsak R, Schöniger E, Ehehalt F, Distler M, Brennand A, Bornstein SR, Weitz J, Solimena M, and Speier S. Dysfunction of Persisting β-Cells is a Key Feature of Early Type 2 Diabetes Pathogenesis. DOI:https://doi.org/10.1016/j.celrep.2020.03.033
New drug combination restores beta cell function in animal model
Targeted pharmacological therapy restores β-cell function for diabetes remission.
Nature Metabolism, 2020
One of the causes of diabetes could be the dedifferentiation of insulin-producing beta cells in the Langerhans' islets of the pancreas, i.e. the loss of cell identity. If and how dedifferentiated beta cells can be targeted by pharmacological intervention for beta cell regeneration is unknown. DZD-Researchers at Helmholtz Zentrum München demonstrated in collaboration with Novo Nordisk for the first time that a targeted combinatorial drug treatment is able to restore beta cell function, achieve beta cell redifferentiation and therefore potentially open new ways for diabetes remission.
To investigate whether dedifferentiated beta cells can be targeted pharmacologically to restore beta cell function, the researchers used streptozotocin-induced diabetes in mice. Using single cell RNA sequencing the researchers could show that after streptozotocin treatment, the surviving beta cells dedifferentiate into a dysfunctional state. The team then tested treatments for their potential to restore beta cell function. The researchers showed that a stable Glucagon-like peptide-1 (GLP-1)/estrogen conjugate (provided by Novo Nordisk) enables targeted and selective delivery of the nuclear hormone cargo to beta cells. The combination of GLP-1/estrogen and a long acting insulin was superior to mono-treatments to both normalize glycemia, glucose tolerance, to increase pancreatic insulin content and to increase the number of beta cells.
This study not only describes the mechanisms of beta cell dedifferentiation and regeneration, , but also reveals pharmacological entry points to target dedifferentiated dedifferentiated beta cells for diabetes remission.
This study brought together scientists from Helmholtz Zentrum München (Helmholtz Diabetes Center and Institute for Computational Biology), the German Center for Diabetes Research (DZD), Technical University Munich (TUM) as well as InSphero AG and Novo Nordisk with the aim to explore the potential therapeutic benefits of GLP1/estrogen treatment in an animal models and in human cells in vitro.
* Streptozotocin is a chemical compound that has a specific toxic effect on insulin-producing beta cells.
Original publication:
Sachs, S. et al, 2020: Targeted pharmacological therapy restores β-cell function for diabetes remission. Nature Metabolism, DOI: 10.1038/s42255-020-0171-3.
Cilia and diabetes: Small cell extension with large effect
Glucose homeostasis is regulated by pancreatic β-cell cilia via endosomal EphA-processing.
Nature Communications, 2019
If the cilia on beta cells of the pancreas do not function properly, glucose intolerance and type 2 diabetes develop. In Nature Communications, a research team from Helmholtz Zentrum München and the German Center for Diabetes Research (DZD) describes the underlying mechanism.
The insulin producing beta cells have primary cilia which are implicated in the regulation of glucose metabolism, insulin signaling and secretion. In order to understand better how these cilia influence the handling of glucose, the researchers removed the cilia from mature beta cells. They found that glucose tolerance and insulin release deteriorated significantly over twelve weeks.
These phenomena were conveyed by special binding sites on beta cells, the ephrin receptors. In this process, EphA/ephrin signals are upregulated, which suppress insulin secretion. Researchers observed similar reactions with islet cells from organ donors. The research group also evaluated data from a small cohort of 19 patients and found a correlation between ciliopathy* genes and blood sugar levels.
"We were able to show in a mouse model that cilia in the pancreas regulate direct pathways of cell-cell communication and thus control blood glucose levels," said Dr. Jantje M. Gerdes. The results of the investigations could provide a basis for future therapies - both for ciliopathies and diabetes.
* Ciliopathies are genetic disorders of the ciliated cell.
Original publication:
F. Volta et al., 2019: Glucose homeostasis is regulated by pancreatic β-cell cilia via endosomal EphA-processing. Nature Communications, doi: 10.1038/s41467-019-12953-5
Type 1 diabetes: defective protection against attack on the body's own cells
miRNA142-3p targets Tet2 and impairs Treg differentiation and stability in models of type 1 diabetes.
Nature Communications, 2019
Regulatory T cells (Tregs) prevent excessive immune reactions in healthy people. In the development of autoimmune type 1 diabetes, this protection is not sufficiently effective. Researchers at the DZD have now deciphered a mechanism that impairs Treg differentiation and stability. The results have now been published in 'Nature Communications'.
Prof. Dr. Carolin Daniel's team was able to decipher a mechanism that leads to the formation of less functional Tregs at an early stage of type 1 diabetes. The microRNA miRNA142-3p plays a decisive role in this process. MicroRNAs can suppress the expression of individual genes. "During the development of autoimmunity in type 1 diabetes, we were able to detect an increased abundance of miRNA142-3p. This leads to a reduced expression of the protein Tet2 in T-helper cells," said Carolin Daniel. As a consequence, faulty epigenetic changes occur in the Foxp3 gene of the regulatory T cells. A decreased number of these important immune cells are formed, and the Tregs are no longer as stable.
New target for future intervention strategies
In order to investigate whether the findings could also open up new therapeutic approaches in the future, the scientists specifically blocked the miRNA142-3p molecule. This improved the formation and stability of the regulatory T cells. In the animal model, the autoimmune response to the insulin-producing beta cells also decreased.
Researchers at the Institute of Diabetes Research (IDF) of Helmholtz Zentrum München, the German Center for Diabetes Research (DZD) and Ludwig-Maximilians-Universität Munich were involved in the studies.
Original publication:
Scherm, M. G. et al. (2019): miRNA142-3p targets Tet2 and impairs Treg differentiation and stability in models of type 1 diabetes. Nature Communications, DOI: 10.1038/s41467-019-13587-3
First Time: Orally Available GLP-1 Agonist More Effective than DPP-IV Inhibitor
With the participation of researchers from the Paul Langerhans Institute Dresden (PLID), a GLP-1 receptor agonist in the form of tablets was compared for the first time with the most common second-line therapy of T2D, a DPP-IV inhibitor. The investigations were carried out in parallel in Japan, France, England, Mexico, Denmark, the USA and Germany as part of the international, randomised double-blind study PIONEER-3. The results are considered to point the way for future therapy of type 2 diabetes.
Patients with diabetes still die 2-3 times more frequently from cardiovascular diseases than people without diabetes. Against this background, so-called incretin analogues have been developed in recent years, i.e. drugs that, like the intestinal hormone GLP-1, lead to the release of insulin in the beta cells of the pancreas and at the same time reduce the feeling of hunger in the brain. "Unfortunately, these drugs, like all peptide-based drugs due to their chemical structure, have to be administered by subcutaneous injection and cannot be taken orally as tablets," said Prof. Dr. Andreas Birkenfeld, PLID, co-author of the study. "Fortunately, the GLP-1 receptor agonist (GLP-1RA) semaglutide is now available as a tablet in combination with an absorption enhancer for the first time."
The 78-week PIONEER-3 study compared 1864 adults with diagnosed type 2 diabetes who took either metformin (with or without sulfonylurea), oral semaglutide in three different doses or sitagliptin (100 mg/d). Oral semaglutide was found to be superior to sitagliptin (at the highest dose) in terms of blood glucose lowering and body weight reduction. The most frequent side effects of GLP-1RA were gastrointestinal effects such as nausea. Although these were more common with semaglutide than with sitagliptin, they are already known from other GLP-1RA and in many cases temporary, so that GLP-1RA are considered safe.
Original publication:
Rosenstock J, Allison D, Birkenfeld AL, Blicher TM, Deenadayalan S, Jacobsen JB, Serusclat P, Violante R, Watada H, Davies M; PIONEER 3 Investigators. Effect of Additional Oral Semaglutide vs Sitagliptin on Glycated Hemoglobin in Adults With Type 2 Diabetes Uncontrolled With Metformin Alone or With Sulfonylurea: The PIONEER 3 Randomized Clinical Trial. JAMA. 2019 Mar 23. doi: 10.1001/jama.2019.2942. [Epub ahead of print]
Link to publication:
https://jamanetwork.com/journals/jama/fullarticle/2729339
Well-regulated Blood Sugar Levels Lower the Risk for Cardiovascular Disease
The regulation of blood glucose should be part of cardiovascular prevention and health promotion measures and be included in evidence-based practice guidelines. This is the result of an extensive systematic umbrella review conducted by DZD researchers at the Paul Langerhans Institute Dresden (PLID) and published in the Journal of the American College of Cardiology (JACC).
Too-high blood sugar (hyperglycemia) as occurs in type 2 diabetes is considered one of the key risk factors for the development of cardiovascular diseases. But how does a blood sugar level that is well regulated by medication or lifestyle changes affect the cardiovascular system? Can this help to prevent diseases of the cardiovascular system such as heart attack or stroke? In order to answer these questions, researchers systematically reviewed current studies on preventive approaches in the field of diabetes and cardiovascular diseases. The analysis was based on three separate systematic literature searches with a total of 2,343 reviews and meta-analyses.
People with type 2 diabetes have a two to three times higher risk of developing cardiovascular disease. The current study shows that well-regulated blood glucose levels through medication can reduce the risk of cardiovascular disease in people with type 2 diabetes. The analysis also shows that individual lifestyle interventions such as a healthy diet and exercise can help to effectively reduce blood sugar levels and thus indirectly lower the risk of cardiovascular disease.
Population-level intervention strategies reduce the risk both directly and indirectly: Physical activity in the workplace helps to avoid dangerous cardiometabolic events. In addition, measures to reduce obesity in people with type 2 diabetes also help to reduce a major risk of cardiovascular disease.
"Our results suggest that it makes sense to develop multicomponent standardized procedures for diabetes prevention and management as well as for the prevention of cardiovascular diseases," said first author Professor Peter Schwarz from the Paul Langerhans Institute Dresden of Helmholtz Zentrum München at the University Hospital Carl Gustav Carus of TU Dresden. The DZD scientist and further authors of the paper suggest that the regulation of blood glucose levels should also be included in evidence-based practice guidelines.
Original publication:
Peter E.H. Schwarz et al. 2018: Blood Sugar Regulation for Cardiovascular Health Promotion and Disease Prevention, JACC Health Promotion Series, Journal of the American College of Cardiology 2018, https://doi.org/10.1016/j.jacc.2018.07.081
How a protein promotes the healing of inflammation
The protein DEL-1, is a central actor that ensures that excessive inflammation subsides. Scientists were able to demonstrate the importance and basic function of this protein. Their work could provide new approaches for the treatment of diseases such as multiple sclerosis, metabolic diseases, inflammatory bone diseases or cancer.
The protein DEL-1, is a central actor that ensures that excessive inflammation subsides. Scientists were able to demonstrate the importance and basic function of this protein. Their work could provide new approaches for the treatment of diseases such as multiple sclerosis, metabolic diseases, inflammatory bone diseases or cancer. The results of the study were now published in the journal "Nature Immunology" (www.nature.com, DOI /10.1038/s41590-018-0249-1).
Inflammatory processes are a natural defense reaction of the immune system against pathogens. Inflammation can spread like a fire and last for a long time if it is not effectively combated. The protein DEL-1 plays a central role in the body's own fire brigade. "We were able to show that DEL-1 decisively regulates the immune defense. Figuratively speaking, the protein controls a large part of the extinguishing and clean-up work. Understanding this mechanism could in future contribute to better treatments for various inflammatory diseases," said Prof. Triantafyllos Chavakis, Director of the Institute of Clinical Chemistry and Laboratory Medicine (IKL) at the TU Dresden and group leader at the Paul Langerhans Institute Dresden.
At the beginning of an inflammatory process, certain immune cells, so-called neutrophils, migrate into the affected tissue. There they drive the inflammation as well as another cell type of the immune defense - so-called macrophages or scavenger cells - which produce inflammation-promoting substances. The protein DEL-1 forms a kind of bridge between macrophages and dying neutrophils. On the one hand, this causes the macrophages to eat dying neutrophils in a kind of clearing up action. On the other hand, DEL-1 reprograms the macrophages to produce anti-inflammatory substances. "Both are important processes that reduce inflammation and restore a healthy balance in the tissue," emphasize Dr. Ioannis Kourtzelis and Dr. Ioannis Mitroulis, scientists at IKL and NCT/UCC Dresden.
"Understanding the mode of action of DEL-1 is an important basis for developing new therapies against metabolic diseases," says DZD-Reseacher Dr. Ünal Coskun of the Paul Langerhans Institute Dresden, which is operated jointly by Helmholtz Zentrum München and the University Hospital at the Technical University of Dresden. Due to its fundamental importance for the inflammatory balance, DEL-1 not only acts as a bridge between immune cells, but also connects research on various diseases.
Original Publication:
Kourtzelis et al. DEL-1 promotes macrophage efferocytosis and clearance of inflammation. Nat Immunol. 2018 Nov 19. doi: 10.1038/s41590-018-0249-1. [Epub ahead of print]
Leptin resistance causes overweight
Many overweight people lack the feeling of being full. It was long thought that this was due to the disrupted transport of the satiety hormone leptin to the brain. That is not the case, as a group of DZD scientists was able to show using a new 3D imaging method. The cause seems to lie in the nerve cells, as the researchers describe in an article in the "International Journal of obesity".
"In obese mice and humans, leptin is released from fatty tissue into the bloodstream in high concentrations but fails to activate the satiety centers in the brain. It has long been assumed that leptin resistance is caused by a disrupted transport process," explains Luke Harrison, a doctoral student at Helmholtz Zentrum München and lead author of the study. As the ability of leptin to cross the blood-brain barrier is limited, so the theory goes, less of it reaches the satiety centers. The innovative 3D technique enabled the researchers to visualize the transport of leptin for the first time and to investigate whether this theory holds up.
Working with biologists, pathologists and structural biologists, Harrison was able to disprove this assumption. Thanks to the new imaging method, the research team headed by Dr. Paul Pfluger, a partner in the German Center for Diabetes Research (DZD), showed that leptin reaches the brain in sufficient quantities both in thin and in obese mice. The cause of the eating disorder must therefore lie in the nerve cells themselves. "We can now narrow down the cause of leptin resistance and focus our research on the molecular mechanisms within nerve cells," says Dr. Paul Pfluger. "
Original publication:
Luke Harrison et. al.: Fluorescent blood brain barrier tracing shows intact leptin transport in obese mice. International Journal of obesity. DOI:10.1038/s41366-018-0221-z
Atlas of Circadian Metabolism
As part of a large-scale study, researchers constructed 24-hour metabolic profiles of mouse tissues and organs under conditions of energy balance and high-fat diet. Their findings provide an overview of how the various metabolic pathways in the body are interconnected and also reveal suitable time frames for anti-obesity therapies. The study was conducted under the aegis of the Helmholtz Zentrum München and the University of California Irvine in collaboration with the German Center for Diabetes Research (DZD). The results have now been published in 'Cell'.
The scientists generated 24 hour metabolic profiles of eight different tissues simultaneously. These included the suprachiasmatic nucleus in the hypothalamus (regarded as the principal circadian pacemaker in mammals), in addition to prefrontal cortex, skeletal muscle, liver, brown and white adipose tissue, blood and sperm.
To understand how diet impacts tissue synchronization and 24 hour metabolism the scientists compared all this data under normal and high-fat diets. High-fat food is known to disrupt circadian rhythms and cause metabolic diseases like obesity and diabetes. This temporal view of tissue metabolism enabled a better insight into how metabolism is changed in metabolic diseases, for example, in the case of obesity and diabetes.
Excess calories from fat upset metabolic rhythms
The researchers were also able to observe how high-fat food consumption disrupts tissue metabolism. In muscle tissue, for instance, they noticed that energy generation from fat and sugar occurred separately and in a very orderly sequence under conditions of energy balance. Under high fat diet, this typical pattern broke down completely and fat metabolism dominated. These changes have major implications for how diet can contribute to development of muscle insulin resistance.
Overall, the study provides an overview of the metabolic processes taking place in the respective tissue at any given time, and also reveals previously unknown links. From that, the authors say, one can also deduce the most promising time frames for administering metabolically effective medication.
Original publication:
Dyar, KA. et al. (2018): Atlas of Circadian Metabolism Reveals System-wide Coordination and Communication between Clocks. Cell, DOI: 10.1016/j.cell.2018.08.042
New Biomarkers of Inflammation Identified as Risk Factors for Neuropathy
Although polyneuropathy is present in about 30% of people with diabetes, it often remains undiagnosed. Scientists from DZD, have now been able to show for the first time that six biomarkers of inflammation indicate the risk of polyneuropathy. The results were published in the current issue of the journal "Diabetes".
Many patients suffer from polyneuropathy, relatively little is currently known about its development, which also limits the therapeutic options. It is known that inflammatory processes contribute to other diabetic complications such as heart attack or stroke. The aim of this new study was therefore the extensive analysis of biomarkers that characterize inflammatory processes as a risk factor for distal sensory polyneuropathy (DSPN). Both people with type 2 diabetes and people in the elderly general population were examined.
Study – Procedure and Design
The study included 513 men and women of the population-based KORA (Cooperative Health Research in the Region of Augsburg) F4/FF4 cohort aged 62 to 81 years who had no distal sensory polyneuropathy at the beginning of the study. Of these individuals, 127 developed a DSPN during the 6.5 year follow-up period. The serum level of 71 biomarkers of inflammation was measured using the new proximity extension assay technology. The serum level of 26 of these 71 biomarkers was higher in people who developed polyneuropathy during the study than in people without polyneuropathy. After statistical correction for multiple testing, higher concentrations of six biomarkers remained associated with the DSPN risk. Three of these proteins (MCP-3/CCL7, MIG/CXCL9, IP-10/CXCL10) were chemokines, while the other three (DNER, CD40, TNFRSF9) were soluble forms of transmembrane receptors.
"In our study, we identified novel biomarkers that indicate the risk of polyneuropathy. For the first time, we were also able to find indications that in addition to the innate immune system, the adaptive immune system could be involved in the development of the disease," said Professor Christian Herder, MD, head of the study at the German Diabetes Center (DDZ).
Original publication:
Herder C, Kannenberg J, Carstensen-Kirberg M, Strom A, Bönhof G, Rathmann W, Huth C, Koenig W, Heier M, Krumsiek J, Peters A, Meisinger C, Roden M, Thorand B, Ziegler D. A Systemic Inflammatory Signature Reflecting Crosstalk Between Innate and Adaptive Immunity Is Associated With Incident Polyneuropathy: KORA F4/FF4 Study. Diabetes. 2018 Aug 16. db180060. DOI: 10.2337/db18-0060 [Epub ahead of print]
Restrictive lung diseases - late consequence of diabetes?
Breathlessness and conditions of restrictive lung disease (RLD), such as pulmonary fibrosis, may be a late complication of type 2 diabetes. These are the key findings of a joint study undertaken by researchers from the German Center for Diabetes Research (DZD) and the German Center for Lung Research (DZL) under the leadership of the University Hospital Heidelberg.
The research team comprised 110 patients with long-term type 2 diabetes, 29 patients with newly diagnosed type 2 diabetes, 68 patients with pre-diabetes and 48 non-diabetic patients (controls). The study participants were examined for metabolic control, diabetes-related complications, breathlessness, and lung function. It was found that people with type 2 diabetes are significantly more likely to suffer from breathlessness and RLD than the control group. RLD was found in 27% of patients with long-term type 2 diabetes, in 20% of patients with newly diagnosed diabetes, and in 9% of patients with pre-diabetes. Patients with pronounced symptoms and RLD also showed CT-morphologically a fibrosating interstitial lung disease. There were also differences in the morphological analysis of the lung tissue of subjects with and without diabetes. Patients with diabetes had increased pulmonary fibrosis. In addition, the study showed that RLD is associated with albuminuria. In the disease, urinary albumin levels are elevated. This may be an indication that lung disease and kidney disease may be associated with diabetic kidney disease (nephropathy).
The researchers suspect that restrictive lung disease (RLD) is a late consequence of type 2 diabetes
Original Publication:
Stefan Kopf, Jan B. Groener, Zoltan Kender, Thomas Fleming, Maik Brune, Christin Riedinger, Nadine Volk, Esther Herpel, Dominik Pesta, Julia Szendrödi, Mark O. Wielpütz, Hans-Ulrich Kauczor, Hugo A. Katus, Michael Kreuter, Peter P. Nawroth. Breathlessness and Restrictive Lung Disease: An Important Diabetes-Related Feature in Patients with Type 2 Diabetes. Respiration 2018, DOI: 10.1159/000488909
New adipokine promotes insulin resistance
In cases of severe obesity, visceral fat cells release a protein that promotes insulin resistance and chronic inflammation. This was discovered by an international team led by scientists from the German Center for Diabetes Research (DZD).
The researchers were able to show for the first time how the protein molecule Wingless-type signaling pathway protein-1 (WISP1) directly impairs the insulin effect in muscle cells and in the liver and thus leads to insulin insensitivity.
The study shows that WISP1 cancels insulin-induced inhibition of glucose production (gluconeogesis) in murine hepatocytes and glycogen synthesis in human muscle cells. The synthesis quantity of the WISP1 protein correlates with the blood glucose levels in the oral glucose tolerance test (OGTT) and with the circulating level of heme oxygenase-1 (HO-1), an enzyme that promotes systemic inflammation, especially in obesity.
The researchers suspect that an increased production of WISP1 from the abdominal fat could be one of the reasons why overweight people often have a disturbed glucose metabolism.
Orginal puplication:
Hörbelt, T., Tacke, C., Markova, M. et al. (2018): The novel adipokine WISP1 associates with insulin resistance and impairs insulin action in myotubes and hepatocytes. Diabetologia https://doi.org/10.1007/s00125-018-4636-9
Increased Glucagon Secretion Not Indispensable Prerequisite for the Development of Diabetes
Only one subgroup of type 2 diabetes (T2D) has elevated glucagon levels. This is the finding of a study conducted by DZD researchers in Munich. The scientists studied glucagon levels in young women with different levels of risk for T2D during an oral glucose tolerance test*. They discovered four patterns of glucagon dynamics that did not match the metabolic phenotypes. The results have now been published in the “Journal of Clinical Endocrinology & Metabolism”.
It is known that glucagon is the main antagonist of insulin, but just what role the hormone plays in the onset of type 2 diabetes is still under debate among scientists. A research team compared glucagon secretion in young women with three different metabolic phenotypes during an oral glucose tolerance test. The groups were: a healthy control group (93 women), metabolically healthy women after gestational diabetes (high-risk group for type 2 diabetes, 121 women) and 71 women who were newly diagnosed with diabetes or prediabetes.
The analysis showed that there are four patterns of glucagon dynamics but that the found patterns did not match the three different metabolic groups. However, one pattern – elevated fasting glucagon levels with delayed glucagon suppression – was particularly common in women with diabetes and prediabetes (21 percent), but this cluster was also discovered in 8 percent of healthy women. Conversely, the majority of women in the prediabetes / diabetes group (n = 39; 55%) had glucagon levels in the normal range with low fasting glucagon and rapid suppression. In addition, in the cluster of high fasting glucagon and poor glucagon suppression, there were increased symptoms of metabolic syndrome (high blood pressure, visceral obesity, and high blood lipids).
The authors of the study therefore assume that increased glucagon secretion in a subgroup can contribute to the development of type 2 diabetes, but this is not an indispensable prerequisite for the development of diabetes.
The study of the DZD, the Medical Center of the University of Munich and Helmholtz Zentrum München was published in the March issue of Journal of Clinical Endocrinology & Metabolism.
Original Publication:
Gar, C. et al. (2018): Patterns of Plasma Glucagon Dynamics Do Not Match Metabolic Phenotypes in Young Women. J Clin Endocrinol Metab; DOI: 10.1210/jc.2017-02014
*Background Information:
Oral Glucose Tolerance Test (oGTT)
The oGTT provides evidence of the body's ability to break down a defined amount of glucose within a given period of time. For this purpose, 75 g of glucose are consumed as a sugar solution on an empty stomach. Subsequently, blood is taken at certain intervals and tested for sugar content.
Visualization of the function of the insulin receptor
Insulin was discovered almost 100 years ago. Now, a German-American research team with DZD involvement was able to show how the hormone activates its receptor. The results and images have been published in the' Journal of Cell Biology'.
Insulin is an important hormone for metabolism in the human body. It is mainly used to channel glucose from the blood into the cells. The hormone acts as a key that opens the cells for the glucose molecules. Insulin docks to the insulin receptors on the cell surface. The receptors then change their shape on the inside of the cell to transmit the signal. However, the exact nature of the structural change has not been known so far.
In order to gain an insight into receptor activation, the researchers have purified complete human insulin receptors and embedded them in nanodiscs. These are disk-shaped miniature membranes, which are just a few nanometers in size and could be made visible directly under the electron microscope. They were able to observe the insulin receptor in an artificial membrane and its structural changes.
In the absence of insulin, the receptor exhibits an inverted U-shaped ectodomain conformation and well-separated transmembrane domains. Insulin binding results in structural rearrangements of the receptor. The receptor takes on a T-shaped structure that allows the transmembrane domains to come together. That's probably what triggers the signal transmission.
“These nanodisc-embedded receptors provide a novel platform to address further questions regarding insulin receptor regulation and eventually to test therapeutic agents”, said Dr. Ünal Coskun, co-senior author of the study and group leader at the DZD - Paul-Langerhans-Institute Dresden of the Helmholtz-Zentrum München at the University Hospital and the Medical Faculty Carl Gustav Carus of the TU Dresden.
Researchers from PLID and Rockefeller University collaborated on the study.
Original-Publication:
Gutmann, Kim et al. (2018): Visualization of ligand-induced transmembrane signaling in the full-length human insulin receptor. Journal of Cell Biology, DOI: 10.1083/jcb.201711047
Largest collection of islet cells reveals new diabetes genes
Systems biology of the IMIDIA biobank from organ donors and pancreatectomised patients defines a novel transcriptomic signature of islets from individuals with type 2 diabetes.
Diabetologia, 2017
A collaborative study has identified a novel cluster of dysregulated genes in the pancreatic islets of patients with type 2 diabetes. The study is part of the EU-Innovative Medicine Initiative (IMI) research consortium IMIDIA.
The goal of the IMIDIA consortium, which involved 14 European academic institutions, large pharma companies and biotech firms from 2010 to 2016, was to identify novel pathways for the regeneration, maintenance and protection of insulin-producing pancreatic beta cells as a mean to expedite the discovery of more effective strategies to prevent and treat diabetes. A main task of the study led by Prof. Michele Solimena, DZD-Speaker, was to define which genes are abnormally expressed in islets of diabetic subjects compared to islets of non-diabetic subjects. The altered expression of these genes could account for beta cell failure in diabetes.
For the first time, the investigators based their comparative gene expression analysis not only on islets collected from non-diabetic and diabetic organ donors, for which the availability of clinical information is limited, but also on islets from patients undergoing pancreatic surgery. The investigators identified nineteen genes the expression of which was altered in islets of both diabetic organ donors as well as diabetic surgical patients. Notably, nine of these nineteen genes had never been shown previously to be dysregulated in diabetic islets. On the other hand, the study could not find evidence for any of these genes to be dysregulated in islets of prediabetic subjects, hence suggesting that their altered expression is a consequence rather than the cause of beta cell failure in diabetes.
Original publication:
Solimena et al., Systems biology of the IMIDIA biobank from organ donors and pancreatectomised patients defines a novel transcriptomic signature of islets from individuals with type 2 diabetes. Diabetologia. 2017 Nov 28. doi: 10.1007/s00125-017-4500-3.
Insulin pump therapy is associated with reduced risks of short-term diabetes complications
Among young patients with type 1 diabetes, insulin pump therapy, compared with insulin injection therapy, was associated with lower risks of severe hypoglycemia and diabetic ketoacidosis and with better glycemic control during the most recent year of therapy. These are the results of a population-based cohort study published in the „Journal of the American Medical Association“.
JAMA, 2017
Type 1 diabetes is the most common metabolic disease in children and adolescents. Insulin pump therapy may improve metabolic control in young patients with type 1 diabetes, but the association with short-term diabetes complications is unclear. Are the rates of severe hypoglycemia and diabetic ketoacidosis lower with insulin pump therapy than with insulin injection therapy in young patients with type 1 diabetes?
To answer these questions researcher conducted a population-based observational study between January 2011 and December 2015 in 350 diabetes centers in Germany, Austria, and Luxembourg. Patients using pump therapy (n = 9814) were matched with 9814 patients using injection therapy.
The Findings: In this population-based observational study including 30 579 young patients with type 1 diabetes, pump therapy, compared with injection therapy, was associated with significantly lower rates of severe hypoglycemia (9.55 vs 13.97 per 100 patient-years) and ketoacidosis (3.64 vs 4.26 per 100 patient-years), and with lower hemoglobin A1c levels (8.04% vs 8.22%) in a propensity score–matched cohort. Also total daily insulin doses were lower for pump therapy compared with injection therapy (0.84 U/kg vs 0.98 U/kg1). There was no significant difference in body mass index between both treatment regimens.
Original publication:
Beate Karges et al: Association of Insulin Pump Therapy vs Insulin Injection Therapy With Severe Hypoglycemia, Ketoacidosis, and Glycemic Control Among Children, Adolescents, and Young Adults With Type 1 Diabetes. JAMA 2017; DOI:10.1001/jama.2017.13994
Elevated hepatic DPP4 activity promotes non-alcoholic fatty liver disease
Elevated hepatic DPP4 activity promotes insulin resistance and non-alcoholic fatty liver disease. Molecular Metabolism, 2017
Increased hepatic expression of dipeptidyl peptidase 4 (DPP4) is associated with non-alcoholic fatty liver disease (NAFLD). Whether this is causative for the development of NAFLD is not yet clarified. DZD-researchers investigate the effect of hepatic DPP4 overexpression on the development of liver steatosis in a mouse model of diet-induced obesity.
In mice that are given a high-fat diet, an increased production of the enzyme DPP4* by the liver promotes an increase in body fat, the development of fatty liver disease and insulin resistance. These were the findings of a current study by DZD-researchers in Potsdam and Tübingen."In combination with our observations from additional human and cell studies, these results indicate that increased DPP4 production by the liver is the cause rather than the consequence of a fatty liver and insulin resistance," says the head of the study, Annette Schürmann from the German Institute for Human Nutrition Research (DIfE), a partner of the German Center for Diabetes Research (DZD). The research team led by Schürmann has now published its findings in Molecular Metabolism.
Original publication:
Christian Baumeier et al: Elevated hepatic DPP4 activity promotes insulin resistance and non-alcoholic fatty liver disease. Molecular Metabolism 2017; DOI: 10.1016/j.molmet.2017.07.016
Fetuin-A leads to pathological changes of the kidney
The protective effect of human renal sinus fat on glomerular cells is reversed by the hepatokine fetuin-A. Scientific Reports 7, 2017
Adipose tissue is not harmful per se. It can even have protective effects. For example, adipose tissue located around blood vessels or the kidney has regenerative properties. "The factor that leads to pathological changes is fetuin-A, which is produced by the fatty liver," said Professor Dorothea Siegel-Axel, DZD scientist at the Institute for Diabetes Research and Metabolic Diseases (IDM) of the Helmholtz Zentrum München at the Eberhard-Karls-University of Tuebingen.
As a result, instead of protecting tissue as before, the adipose tissue now elicits inflammatory processes. This leads to a restriction of renal function. This is demonstrated by studies on arteries and the kidney, which have recently been published by the working group in the journal Scientific Reports (Nature Group).
Background: DZD scientists in Tuebingen discovered several years ago that especially a fatty liver can cause damage to other organs. The cause for this is the altered secretion behavior of the fatty liver. It increasingly produces glucose, unfavorable fats and proteins, such as the hepatokine fetuin-A, all of which it releases into the bloodstream. Thus, the secreted substances of the fatty liver enter other organs and trigger reactions there (organ crosstalk).
Original publication:
Wagner R. et al (2017): The protective effect of human renal sinus fat on glomerular cells is reversed by the hepatokine fetuin-A. Scientific Reports, DOI: 10.1038/s41598-017-02210-4
Insulin in the Brain Influences the Metabolism in the Body
Hypothalamic and striatal insulin action suppresses endogenous glucose production and may stimulate glucose uptake during hyperinsulinemia in lean but not in overweight men. Diabetes, 2017
Insulin acts in certain regions of the human brain. If the hormone is administered via an intranasal spray, the insulin is delivered to the brain directly. In lean people, the administration of intranasal insulin results in an improvement of insulin action in the whole body by suppressing endogenous glucose production, causing more glucose to be absorbed by the tissue. In overweight subjects these effects did not occur. These were the results of a study by DZD scientists from Tübingen and Düsseldorf, which was published in the journal Diabetes.
In order to measure the endogenous glucose production and the glucose uptake of the tissue, the 21 study participants underwent two hyperinsulinemic-euglycemic clamps with labeled glucose infusion (method for determining insulin sensitivity). In addition, the participants were administered an intranasal insulin spray or a placebo spray. The researchers investigated brain activity by means of functional magnetic resonance tomography (fMRI).
After the insulin administration, the endogenous glucose production decreased and glucose uptake in the tissue increased in the lean subjects. In addition, the researchers also observed increased activity in the hypothalamus and striatum (part of the basal ganglia, which belong to the cerebrum). No such effects were detected in the overweight participants. This could be due to insulin resistance in the brain of overweight people, which has been known for some time. This insulin resistance of the brain consequently has negative effects on the metabolism in the body, the researchers suspect.
The study was conducted by the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen and the German Diabetes Center in Düsseldorf, both partners of the German Center for Diabetes Research (DZD).
Original publication:
Martin Heni, Robert Wagner, Stephanie Kullmann, Sofiya Gancheva, Michael Roden, Andreas Peter, Norbert Stefan, Hubert Preissl, Hans Ulrich Haring, Andreas Fritsche. Hypothalamic and striatal insulin action suppresses endogenous glucose production and may stimulate glucose uptake during hyperinsulinemia in lean but not in overweight men. Diabetes, 2017; db161380. https://doi.org/10.2337/db16-1380
mIndy affects hepatic lipid metabolism
The Human Longevity Gene Homolog INDY and Interleukin-6 Interact in Hepatic Lipid Metabolism. Hepatology, 2017
Reduced expression of the Indy (‘I am Not Dead, Yet') gene in lower organisms promotes longevity in a manner akin to caloric restriction. The mammalian homolog of Indy (mIndy, Slc13a5) affects hepatic lipid metabolism. In obese, insulin resistant patients with NAFLD, hepatic mIndy expression was increased and mIndy expression was also independently associated with hepatic steatosis.
Liver microarray analysis showed that high mIndy expression was associated with pathways involved in hepatic lipid metabolism and immunological processes. Interleukin-6 (IL-6) was identified as a regulator of mIndy by binding to its cognate receptor. Studies in human primary hepatocytes confirmed that IL-6 markedly induced mIndy transcription. Activation of the IL-6-Stat3 pathway stimulated mIndy expression, enhanced cytoplasmic citrate influx and augmented hepatic lipogenesis in vivo. These data show that mIndy is increased in liver of obese humans and non-human primates with NALFD. Targeting human mINDY may have therapeutic potential in obese patients with NAFLD.
Orignal publication:
von Loeffelholz et al., The Human Longevity Gene Homolog INDY and Interleukin-6 Interact in Hepatic Lipid Metabolism, Hepatology 2017 http://dx.doi.org/10.1002/hep.29089
People with prediabetes should avoid high-Carbohydrate Foods in the evening
The effect of diurnal distribution of carbohydrates and fat on glycaemic control in humans: a randomized controlled trial. Scientific Reports 7, 2017
The internal clock influences how people with impaired glucose metabolism react to carbohydrate-rich food. Men with prediabetes, abundant consumption of foods containing starch and sugar in the evening had a negative effect on their blood glucose regulation. These are the results of a nutrition study led by the German Institute of Human Nutrition (DIfE).
Furthermore, in the affected men the researchers observed an altered secretion of the intestinal hormones glucagon-like peptide-1 (GLP-1) and peptide YY (PYY), which contribute to the regulation of the glucose metabolism or body weight and whose secretion is subject to a particular circadian rhythm. Thus, the blood levels of the two hormones decreased significantly parallel to the pronounced decrease of glucose tolerance in the afternoons in the affected persons in contrast to the healthy participants.
“The circadian rhythm of the hormonal release thus influences the way we react to carbohydrates,” said endocrinologist Pfeiffer, who heads the Department of Clinical Nutrition at DIfE.
Original publication:
Kessler, K. et al. The effect of diurnal distribution of carbohydrates and fat on glycaemic control in humans: a randomized controlled trial. Sci. Rep. 7, 44170; doi: 10.1038/srep44170 (2017).
Pancreas lineage allocation and specification are regulated by S1p
Pancreas lineage allocation and specification are regulated by sphingosine-1-phosphate signalling.
PLoS Biol., 2017
Sphingosine-1-phosphate has a key role in mouse pancreas progenitor survival and the generation of the endocrine and acinar lineages. S1p signaling promotes endocrine specification by stabilizing YAP and attenuating Notch signaling.
The pancreas develops from a field of progenitor cells localised in a restricted region of the embryonic endoderm. These progenitor cells proliferate and eventually differentiate to generate the three distinct lineages comprising the endocrine (which include insulin-producing β cells), acinar, and ductal cells. DZD-Reseachers show that a phospholipid, sphingosine-1-phosphate (S1p), generated by the progenitor cells themselves, acts as a signal necessary to define the acinar and endocrine lineage. They observe that in the absence of S1p only duct cells are generated and the survival of pancreas progenitors is compromised.
The function of this signalling pathway in the generation of the endocrine cells is two-fold. Firstly, it stabilizes yes-associated protein (YAP), a transcriptional gene coactivator known to regulate pancreatic progenitor proliferation. The reseachers show that this stability is necessary for the activation of the endocrine specification program. Secondly, it attenuates Notch signalling, allowing the generation of endocrine and acinar cells. Notch attenuation is necessary for the stabilisation of the transcription factor Ngn3, which is required for the generation of endocrine cells.
The DZD-Reseachers conclude that S1p acts as an autocrine signal regulating YAP stabilization and Notch attenuation to mediate pancreas specification. Understanding lineage allocation and specification in the pancreas will shed light on the origins of pancreatic diseases and may suggest novel therapeutic approaches.
Original publication:
Serafimidis I., Rodriguez-Aznar E., Lesche M., Yoshioka K., Takuwa Y., Dahl A., Pan D., Gavalas A.
Pancreas lineage allocation and specification are regulated by sphingosine-1-phosphate signalling.
PLoS Biol. 2017 Mar 1;15(3):e2000949. doi: 10.1371/journal.pbio.2000949. eCollection 2017.
Even One High-Fat Meal Can Harm the Metabolism
Acute dietary fat intake initiates alterations in energy metabolism and insulin resistance. Journal of Clinical Investigation, 2017
A single ingestion of a large quantity of palm oil suffices to reduce the body's sensitivity to insulin and also to induce increased fat deposits and changes in the energy metabolism of the liver.
DZD researchers from the German Diabetes Center, together with scientists from Helmholtz Zentrum München and Portuguese colleagues, have published a study in "The Journal of Clinical Investigation" on the effects of high-fat intake in healthy, lean male participants. Each participant randomly received a flavored palm oil drink or a glass of clear water as a control experiment. The palm oil drink contained a similar amount of saturated fat as two cheeseburgers with bacon and a large portion of French fries or two pepperoni pizzas. The scientists showed that this single high-fat meal sufficed to reduce the insulin action, i.e., to induce insulin resistance and to increase the fat content of the liver. In addition, alterations in the energy metabolism of the liver were detected. The observed metabolic changes are similar to the changes observed in people with type 2 diabetes or non-alcoholic fatty liver disease (NAFLD).
The study results provide information about the earliest alterations in the liver metabolism, which in the case of overweight and diabetes can, over the long term, lead to fatty liver diseases.
Original publication:
Elisa Álvarez Hernández, Sabine Kahl, Anett Seelig, Paul Begovatz, Martin Irmler, Yuliya Kupriyanova, Bettina Nowotny, Peter Nowotny, Christian Herder, Cristina Barosa, Filipa Carvalho, Jan Rozman, Susanne Neschen, John G. Jones, Johannes Beckers, Martin Hrabě de Angelis and Michael Roden, Acute dietary fat intake initiates alterations in energy metabolism and insulin resistance, J Clin Invest. 2017., 23. Januar 2017. doi:10.1172/JCI89444.
Correlative light and electron microscopy for quantitative studies
A Global Approach for Quantitative Super Resolution and Electron Microscopy on Cryo and Epoxy Sections Using Self-labeling Protein Tags. Scientific Reports 7, 2017
Correlative light and electron microscopy (CLEM) is a powerful approach to investigate the molecular ultrastructure of labeled cell compartments. However, quantitative CLEM studies are rare, mainly due to small sample sizes and the sensitivity of fluorescent proteins to strong fixatives and contrasting reagents for EM. DZD-Reseachers show that fusion of a self-labeling protein to insulin allows for the quantification of age-distinct insulin granule pools in pancreatic beta cells by a combination of super resolution and transmission electron microscopy on Tokuyasu cryosections. In contrast to fluorescent proteins like GFP organic dyes covalently bound to self-labeling proteins retain their fluorescence also in epoxy resin following high pressure freezing and freeze substitution, or remarkably even after strong chemical fixation. This enables for the assessment of age-defined granule morphology and degradation. Finally, we demonstrate that this CLEM protocol is highly versatile, being suitable for single and dual fluorescent labeling and detection of different proteins with optimal ultrastructure preservation and contrast.
Figure:
F.l.: (a) SIM image of Epon section of SOFIA mouse beta cells labeled with 505-Star (green) and TMR-Star (magenta) fixed by HPF followed by FS. As fiducial markers fluorescent beads (blue) were added to the section prior to imaging. Punctate SGs can be unequivocally distinguished by SIM. (b) CLEM image of boxed area in (a). (c) CLEM detail of boxed area in (c) showing perfect overlay of 505+ and TMR+ SGs. Scale bars: (a) 10 µm. (b+c) 1 µm.
Original publication:
Andreas Müller, Martin Neukam, Anna Ivanova, Anke Sönmez, Carla Münster, Susanne Kretschmar, Yannis Kalaidzidis, Thomas Kurth, Jean-Marc Verbavatz & Michele Solimena. A Global Approach for Quantitative Super Resolution and Electron Microscopy on Cryo and Epoxy Sections Using Self-labeling Protein Tags. Scientific Reports 7, Article number: 23 (2017). doi:10.1038/s41598-017-00033-x
Overweight Affects DNA Methylation
Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature 2016
High BMI leads to epigenetic changes at nearly 200 loci of the genome – with effects on gene expression. This is the result of a large-scale international study coordinated by Helmholtz Zentrum München, a partner in the German Center for Diabetes Research.
An international research team led by Dr. Christian Gieger and Dr. Harald Grallert (as well as Jaspal Kooner and John Chambers of Imperial College London) examined possible correlations between body mass index (BMI) and epigenetic changes.
The scientists examined the blood samples of over 10,000 women and men from Europe. A large proportion of these were inhabitants of London of Indian ancestry, who according to the authors are at high risk for obesity and metabolic diseases. In a first step with 5,387 samples, the research team identified 207 gene loci that were epigenetically altered dependent on the BMI. They then tested these candidate loci in blood samples of an additional 4,874 subjects and were able to confirm 187 of these. Further studies and long-term observations also indicated that the changes were predominantly a consequence of being overweight – not the cause.
Significant changes were found in the expression of genes responsible for lipid metabolism and substrate transport, but inflammation-related gene loci were also affected. From the data, the team was also able to identify epigenetic markers that could predict the risk of type 2 diabetes.
Original publication:
Wahl, S. et al. (2016): Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature, doi:10.1038/nature20784
Friendly Fire in the Pancreas
miRNA92a targets KLF2 and PTEN signaling to promote human T follicular helper precursors in T1D islet autoimmunity.
PNAS, 2016
Type 1 diabetes is an autoimmune disease in which the body destroys its own beta cells in the pancreas. Researchers are still seeking to find out what causes this malfunction of the immune system in order to intervene therapeutically in the processes. A team led by Dr. Carolin Daniel, group leader at the Institute of Diabetes Research (IDF) of Helmholtz Zentrum München, has now discovered a further piece in solving this puzzle.
“For the first time, we were able to show that in the affected children an increased number of specific immune cells are found in the blood at the beginning of the autoimmune response,” said Daniel. She and her team had previously analyzed blood samples of children in a biobank established by Professor Anette-Gabriele Ziegler, director of the IDF, within the framework of large-scale cohort studies.
According to the authors, these special immune cells are so-called insulin-specific T follicular helper cells (TFH). They appear in the lymph nodes, among other organs, and initiate attacks of the immune system by promoting the production of antibodies by B cells. Now the scientists have found increased frequencies of these cells in samples of children with recent onset of islet cell autoimmunity – an early stage of type 1 diabetes.
In the search for the causes of the increase in TFH cells during autoimmune activation in children, the scientists discovered a previously unknown signaling pathway. The analyses showed that a molecule called miRNA92a triggers a chain of molecular events, which ultimately leads to the increase in these immune cells.
To check whether this newly discovered mechanism is suitable for therapeutic intervention, the scientists investigated the effect of a so-called antagomir, which specifically binds to miRNA92a molecules and blocks their effect. In an experimental model of type 1 diabetes and in the humanized model, this treatment resulted in a significantly lower autoimmune response. (see figure: Treatment with an antagomir directed against miR92a results in reduced attacks of immune cells (green) on the insulin (white) producing beta cells directly in the pancreas. Moreover, the treatment leads to more regulatory T cells (red) able to protect the beta cells.)
Original publication:
Serr, I. et al. (2016). miRNA92a targets KLF2 and PTEN signaling to promote human T follicular helper precursors in T1D islet autoimmunity, DOI: 10.1073/pnas.160664611
High-Protein Diets Reduce Liver Fat
Isocaloric Diets High in Animal or Plant Protein Reduce Liver fat and Inflammation in Individuals with Type 2 Diabetes.
Gastroenterology 2016
According to a new nutritional study conducted by the German Institute of Human Nutrition (DIfE) on individuals with type 2 diabetes, high-protein diets reduced liver fat by up to 48 percent within six weeks. It did not matter whether the diet was mainly based on plant or animal protein.
Nonalcoholic fatty liver disease is the most common chronic liver disease in Europe and the U.S. “When left untreated, fatty liver is an important step progress to type 2 diabetes and can develop into liver cirrhosis, which can have life-threatening effects,” said endocrinologist Andreas F. H. Pfeiffer of DIfE, who led the study. "Since the number of affected persons is increasing, it is therefore more important than ever to work together with our partners to develop effective dietary strategies that prevent the disease," he added.
Researchers at DIfE investigated in the current study the effects of two high-protein diets on the metabolism of 37 female and male subjects between the ages of 49 and 78 years suffering from type 2 diabetes and, in most cases, from fatty liver. The two diets differed only in the protein sources, which were either mainly plant or animal origin.
The results: All study participants benefited from the high-protein diet, whether based on plant or animal protein. Liver fat content decreased significantly, in half of the study participants by more than 50 percent. Negative effects on renal function or glucose metabolism were not observed.
The team of scientists led by Mariya Markova, Olga Pivovarova, Silke Hornemann and Andreas F. H. Pfeiffer of DIfE, a partner of the German Center for Diabetes Research (DZD), has published its findings in the journal "Gastroenterology".
Original publication:
Markova et al. 2016. Isocaloric Diets High in Animal or Plant Protein Reduce Liver fat and Inflammation in Individuals with Type 2 Diabetes, Gastroenterology 2016. DOI: http://dx.doi.org/10.1053/j.gastro.2016.10.007
Calcineurin: Key molecule in energy metabolism
Pfluger PT, Kabra DG, Aichler M, Schriever SC, Pfuhlmann K, García VC, Lehti M, Weber J, Kutschke M, Rozman J, Elrod JW, Hevener AL, Feuchtinger A, Hrabě de Angelis M, Walch A, Rollmann SM, Aronow B, Müller TD, Perez-Tilve D, Jastroch M, De Luca M, Molkentin JD, Tschöp MH. Calcineurin Links Mitochondrial Elongation with Energy Metabolism.
doi: 10.1016/j.cmet.2015.08.022. Cell Metabolism. Sep 23, 2015
Our body consistently adjusts its energy management to changes in the supply of nutrients or physical activity. Malfunctioning in this process plays an essential role in the genesis of metabolic disorders like adiposity and diabetes. Scientists at the Helmholtz Zentrum München now report that in this process the protein calcineurin assumes a central function by optimising cellular respiration. Genetic as well as pharmacological calcineurin inhibition protects from diet-induced obesity in both a fly and mouse animal models.
The evolutionary highly conserved role of calcineurin in fly and mouse energy metabolism suggests a similar function in humans. It would therefore be an obvious conclusion to suppress the function of calcineurin through medication in order to treat obesity. Corresponding inhibitors have been deployed in high dosages in the clinic for years in order to prevent rejection reactions after tissue transplants but due to numerous side effects have not been above criticism. Effects from low-dosage calcineurin inhibitors on the body weight of adipose patients have, however, not yet been studied clinically. Corresponding new approaches are currently being tested. They could play a role in future diabetes therapies.
Original publication:
Pfluger PT, Kabra DG, Aichler M, Schriever SC, Pfuhlmann K, García VC, Lehti M, Weber J, Kutschke M, Rozman J, Elrod JW, Hevener AL, Feuchtinger A, Hrabě de Angelis M, Walch A, Rollmann SM, Aronow B, Müller TD, Perez-Tilve D, Jastroch M, De Luca M, Molkentin JD, Tschöp MH. Calcineurin Links Mitochondrial Elongation with Energy Metabolism. doi: 10.1016/j.cmet.2015.08.022. Cell Metabolism. Sep 23, 2015
Link to the publication:
http://www.sciencedirect.com/science/article/pii/S1550413115004556
Diabetes prevention: Who benefits from lifestyle modification?
Stefan N, Staiger H, Wagner R, Machann J, Schick F, Häring HU, Fritsche A. A high-risk phenotype associates with reduced improvement in glycaemia during a lifestyle intervention in prediabetes.
doi: 10.1007/s00125-015-3760-z. Diabetologia. September 24, 2015
DZD scientists at the University of Tübingen identified a phenotype among patients with prediabetes that is associated with nonresponse to lifestyle modification in the Tübingen Lifestyle Intervention Program (TULIP). These participants showed a lack of reversal of prediabetes (impaired glucose tolerance and/or impaired fasting glucose) to normal glucose regulation (NGR) despite reduction of body weight. Characteristics of non-responders were low insulin secretion relative to insulin resistance or insulin-resistant nonalcoholic fatty liver disease (= high-risk phenotype). The odds ratio for reaching the status NGR was 4.54 (95% CI 2.08, 9.94) for participants having the low-risk phenotype.
In future, stratification of individuals with prediabetes at baseline into a high-risk and a low-risk phenotype may help to determine the effectiveness of a lifestyle intervention to revert individuals to NGR. The next question is: Can a reduced response to a standard
lifestyle intervention in individuals with the identified high-risk phenotype be overcome by an intensified lifestyle intervention? The German Prediabetes Lifestyle Intervention Study (PLIS) has been started in eight centres throughout Germany to investigate this issue.
Original publication:
Stefan N, Staiger H, Wagner R, Machann J, Schick F, Häring HU, Fritsche A. A high-risk phenotype associates with reduced improvement in glycaemia during a lifestyle intervention in prediabetes. doi: 10.1007/s00125-015-3760-z. Diabetologia. September 24, 2015
Link to the publication:
http://link.springer.com/article/10.1007%2Fs00125-015-3760-z
Study on healthy aging: Knockdown of Indy/CeNac2 extends Caenorhabditis elegans life span
Schwarz F, Karadeniz Z, Fischer-Rosinsky A, Willmes DM, Spranger J, Birkenfeld AL. Knockdown of Indy/CeNac2 extends Caenorhabditis elegans life span by inducing AMPK/aak-2.
Aging. August 20, 2015
DZD scientists of the group of Prof. Andreas Birkenfeld at the University Clinic Carl Gustav Carus, TU Dresden, were able to shed a new light on the controversial data on life span extension in C. elegans.
It has been known that reduced expression of the Indy (“I am Not Dead Yet”) gene in Drosophila melanogaster promotes longevity. Now, the researchers could show that the knockdown of Indy/CeNAC2 using a specific siRNA extended the life span of C. elegans along with the activation of the intracellular energy sensor AMP-activated protein Kinase A (AMPK). Mean life span was extended by 22±3 % upon knockdown of Indy/CeNAC2, while whole body fat content was reduced by nearly 50%. This finding might also be interesting for future diabetes therapies in humans.
The study provides a rationale for the molecular mechanisms mediating longevity when Indy/CeNAC2 is reduced. It further supports the hypothesis that activation of AMPK and inactivation of Indy are attractive targets to promote healthy ageing and, possibly, to extend life span also in higher eukaryotes.
Original publication:
Schwarz F, Karadeniz Z, Fischer-Rosinsky A, Willmes DM, Spranger J, Birkenfeld AL. Knockdown of Indy/CeNac2 extends Caenorhabditis elegans life span by inducing AMPK/aak-2. Aging. August 20, 2015 Link to the Publication
www.impactaging.com/papers/v7/n8/full/100791.html
Stool microbiota of high-risk people for type 2 diabetes
Fugmann M, Breier M, Rottenkolber M, Banning F, Ferrari U, Sacco V, Grallert H, Parhofer KG, Seissler J, Clavel T, Lechner A. The stool microbiota of insulin resistant women with recent gestational diabetes, a high risk group for type 2 diabetes. doi: 10.1038/srep13212.
Nature Scientific Reports. August 17, 2015
The gut microbiota influences metabolic health and has already been linked to diabetes. DZD scientist from Munich now investigated the microbiome of young adults at risk for type 2 diabetes. They compared stool microbiota of insulin resistant women with previous gestational diabetes – a high risk group for type 2 diabetes – and women after a normoglycemic pregnancy (controls).
Significantly more women in the previous gestational diabetes group showed a Prevotellaceae-dominated intestinal microbiome. Prevotella are mucin degrading bacteria, which may be associated with increased gut permeability and low-grade inflammation with decreased insulin sensitivity. This could explain the link between Prevotellaceae and diabetes.
The study suggests that distinctive features of the intestinal microbiota are already present
in young adults at risk for type 2 diabetes. These results warrant further investigation in larger human cohorts and other clinical settings, as well as examination of the underlying molecular mechanisms. Considering that the gut microbiota can be influenced by diet, this might be a suitable way to prevent type 2 diabetes in people at risk.
Original publication:
Fugmann M, Breier M, Rottenkolber M, Banning F, Ferrari U, Sacco V, Grallert H, Parhofer KG, Seissler J, Clavel T, Lechner A. The stool microbiota of insulin resistant women with recent gestational diabetes, a high risk group for type 2 diabetes. doi: 10.1038/srep13212. Nature Scientific Reports. August 17, 2015
Link to the publication:
http://www.nature.com/articles/srep13212
New diabetes-related genes discovered
Hrabě de Angelis, M. et al. Analysis of mammalian gene function through broad-based phenotypic screens across a consortium of mouse clinics.
Nature Genetics. doi: 10.1038/ng.3360. September 1, 2015
The role of 300 genes has been revealed by DZD scientists in cooperation with colleagues of the European Mouse Disease Clinic (EUMODIC) to understand the part they play in disease and biology. In order to study gene function, they analyzed mouse lines which each had a single gene removed. 160 disease-related genes were discovered. Some of them play a role in diabetes and are promising candidates for further diabetes research.
EUMODIC was the first step towards the creation of a database of all mouse gene functions, a vision now being realized by the International Mouse Phenotyping Consortium (IMPC). The published data set is available on the IMPC website for other scientists to use it in their own research. This will allow to understand more about genes we currently know very little about, and open up new ways for research into the genetics of human disease.
Original publication:
Hrabě de Angelis, M. et al. Analysis of mammalian gene function through broad-based phenotypic screens across a consortium of mouse clinics. Nature Genetics. doi: 10.1038/ng.3360. September 1, 2015
Link to the publication:
http://www.nature.com/ng/journal/v47/n9/full/ng.3360.html
New surgically reversible diabetes subtype
Ehehalt F, Sturm D, Rösler M, Distler M, Weitz J, Kersting S, Ludwig B, Schwanebeck U, Saeger HD, Solimena M, Grützmann R. Blood Glucose Homeostasis in the Course of Partial Pancreatectomy – Evidence for Surgically Reversible Diabetes Induced by Cholestasis.
doi: 10.1371/journal.pone.0134140.
PLoS One. August 6, 2015
DZD scientists at the Paul Langerhans Institute Dresden characterized a new reversible, tumor-associated diabetes subtype: Cholestasis-induced diabetes. This surgically reversible blood glucose dysregulation diagnosed concomitantly with a (peri-)pancreatic tumor appears secondary to compromised liver function due to tumor compression of the common bile duct and the subsequent increase in insulin resistance.
Individuals undergoing elective partial pancreatic resection were recruited into this trial. They were assigned into three groups: deteriorated, stable or improved glucose homeostasis three months after surgery.
Stability and improvement of glucose homeostasis were associated with tumor resection and postoperative normalization of recently diagnosed glucose dysregulation, preoperatively elevated tumor markers and markers for common bile duct obstruction, acute pancreatitis and liver cell damage.
These data enable the pancreatic surgeon to estimate the postoperative metabolic consequences in the course of partial pancreatic resection and to improve his patient’s information accordingly. Furthermore, “new-onset diabetes” in elderly patients (age >50 years) and temporary surveillance of bile duct, pancreas and liver cell parameters during the first months after the diagnosis of impaired glucose metabolism in the elderly might serve as an effective and practical filter for pancreatic cancer screening.
Original publication:
Ehehalt F, Sturm D, Rösler M, Distler M, Weitz J, Kersting S, Ludwig B, Schwanebeck U, Saeger HD, Solimena M, Grützmann R. Blood Glucose Homeostasis in the Course of Partial Pancreatectomy – Evidence for Surgically Reversible Diabetes Induced by Cholestasis.
doi: 10.1371/journal.pone.0134140. PLoS One. August 6, 2015
Link to the Publication
Positive side effect: Metformin lowers LDL cholesterol levels
Xu T, Brandmaier S, Messias AC, Herder C, Draisma HH, Demirkan A, Yu Z, Ried JS, Haller T, Heier M, Campillos M, Fobo G, Stark R, Holzapfel C, Adam J, Chi S, Rotter M, Panni T, Quante AS, He Y, Prehn C, Roemisch-Margl W, Kastenmüller G, Willemsen G, Pool R, Kasa K, van Dijk KW, Hankemeier T, Meisinger C, Thorand B, Ruepp A, Hrabé de Angelis M, Li Y, Wichmann HE, Stratmann B, Strauch K, Metspalu A, Gieger C, Suhre K, Adamski J, Illig T, Rathmann W, Roden M, Peters A, van Duijn CM, Boomsma DI, Meitinger T, Wang-Sattler R. Effects of Metformin on Metabolite Profiles and LDL Cholesterol in Patients With Type 2 Diabetes. doi: 10.2337/dc15-0658.
Besides affecting the blood sugar levels, the substance Metformin also has an impact on blood fat levels. This was elucidated by an interdisciplinary team of the DZD headed by Dr. Rui Wang-Sattler of the Helmholtz Zentrum München. Especially LDL cholesterol can be reduced.
The DZD-researchers at Helmholtz Zentrum München and German Diabetes Center Düsseldorf analyzed more than 1.800 blood samples of participants, who joined the German large-scale study KORA*. Using a comprehensive approach, the scientists investigated metabolic products (metabolites) as well as genetics of these participants. They found that the administration of Metformin in patients suffering from type 2 diabetes led to a change in metabolite levels. This was associated with a decreased level of LDL cholesterol, which is under strong suspicion to promote cardiovascular diseases by causing atherosclerosis.
The study suggests that Metformin might have an additional beneficial effect with regards to cardiovascular diseases among diabetes patients. The exact mechanism of Metformin will be further investigated.
* For more than 20 years, the Cooperative Health Research in the Region of Augsburg (KORA) has been examining the health of thousands of citizens in Augsburg and environs.
Original publication:
Xu T, Brandmaier S, Messias AC, Herder C, Draisma HH, Demirkan A, Yu Z, Ried JS, Haller T, Heier M, Campillos M, Fobo G, Stark R, Holzapfel C, Adam J, Chi S, Rotter M, Panni T, Quante AS, He Y, Prehn C, Roemisch-Margl W, Kastenmüller G, Willemsen G, Pool R, Kasa K, van Dijk KW, Hankemeier T, Meisinger C, Thorand B, Ruepp A, Hrabé de Angelis M, Li Y, Wichmann HE, Stratmann B, Strauch K, Metspalu A, Gieger C, Suhre K, Adamski J, Illig T, Rathmann W, Roden M, Peters A, van Duijn CM, Boomsma DI, Meitinger T, Wang-Sattler R. Effects of Metformin on Metabolite Profiles and LDL Cholesterol in Patients With Type 2 Diabetes. doi: 10.2337/dc15-0658. Diabetes Care. August 5, 2015
Link to the publication:
http://care.diabetesjournals.org/content/early/2015/07/27/dc15-0658.abstract
Intake of Lactobacillus reuteri improves incretin and insulin secretion
Simon MC, Strassburger K, Nowotny B, Kolb H, Nowotny P, Burkart V, Zivehe F, Hwang JH, Stehle P, Pacini G, Hartmann B, Holst JJ, MacKenzie C, Bindels LB, Martinez I, Walter J, Henrich B, Schloot NC, Roden M. Intake of Lactobacillus reuteri Improves Incretin and Insulin Secretion in Glucose Tolerant Humans: A Proof of Concept. doi: 10.2337/dc14-2690.
Diabetes Care. June 17, 2015
Alterations in gut microbiota occur in obesity and type 2 diabetes. DZD scientists at the German Diabetes Center in Düsseldorf and an international research team analyzed the effects of daily intake of Lactobacillus reuteri. The prospective, double-blind, randomized trial was performed in 21 glucose tolerant humans. L. reuteri increased glucose-stimulatedGLP-1 and GLP-2 release by 76% and 43%, respectively, compared with placebo, along with 49% higher insulin and 55% higher C-peptide secretion. However, the intervention did not alter peripheral and hepatic insulin sensitivity, body mass, ectopic fat content, orcirculating cytokines.
The authors conclude that enrichment of gut microbiota with L. reuteri increases insulin secretion, possibly due to augmented incretin release, but does not directly affect insulin sensitivity or body fat distribution. This suggests that oral ingestion of one specific strain may
serve as a novel therapeutic approach to improve glucose-dependent insulin release.
Original publication:
Simon MC, Strassburger K, Nowotny B, Kolb H, Nowotny P, Burkart V, Zivehe F, Hwang JH, Stehle P, Pacini G, Hartmann B, Holst JJ, MacKenzie C, Bindels LB, Martinez I, Walter J, Henrich B, Schloot NC, Roden M. Intake of Lactobacillus reuteri Improves Incretin and Insulin Secretion in Glucose Tolerant Humans: A Proof of Concept. doi: 10.2337/dc14-2690. Diabetes Care. June 17, 2015
Link to the publication:
http://care.diabetesjournals.org/content/early/2015/05/15/dc14-2690.long
Effects of aging on insulin in the brain
Sartorius T, Peter A, Heni M, Maetzler W, Fritsche A, Häring HU, Hennige AM. The brain response to peripheral insulin declines with age: a contribution of the blood-brain barrier? doi: 10.1371/journal.pone.0126804.
PLoS One. May 12, 2015
DZD scientists at the Institute for Diabetes Research and Metabolic Diseases (IDM) and scientists at the German Center for Neurodegenerative Diseases (DZNE) investigated the effect of aging on insulin concentrations in the periphery and the central nervous system as well as its impact on insulin-dependent brain activity.
In humans, glucose and insulin concentrations in cerebrospinal fluid (CSF) were tightly correlated with the respective serum/plasma concentrations. The CSF/serum ratio for insulin was reduced in older subjects while the CSF/serum ratio for albumin increased with age like for most other proteins. Insulin-mediated cortical brain activity instantly increased in young mice subcutaneously injected with insulin but was significantly reduced and delayed in aged mice during the treatment period. However, when insulin was applied intracerebroventricularly into aged animals, brain activity was readily improved.
An inadequate insulin transport into the central nervous system across the blood-brain barrier may contribute to impaired insulin action in elderly subjects, which finally harms glucose homeostasis and neuronal function. This information is crucial for more efficient preventive and therapeutic interventions like specific insulin sensitizing agents in an aging population.
Original publication:
Sartorius T, Peter A, Heni M, Maetzler W, Fritsche A, Häring HU, Hennige AM. The brain response to peripheral insulin declines with age: a contribution of the blood-brain barrier? doi: 10.1371/journal.pone.0126804. PLoS One. May 12, 2015
Link to the publication:
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0126804
Visualization of digestion and microbial metabolism – better understanding of metabolic diseases
Heinzmann SS, Schmitt-Kopplin P. Deep metabotyping of the murine gastrointestinal tract for the visualization of digestion and microbial metabolism. doi: 10.1021/acs.jproteome.5b00034.
J Proteome Res. May 1, 2015
Obesity and diabetes are influenced by gastrointestinal metabolism. To gain a better understanding of the interdependencies DZD scientists at the Helmholtz Zentrum München analyzed the metabolic and physiological functions of different sections of the gut. The aim was to define a comprehensive list of characteristic metabolites for the physiological gut sections and to quantify the selected pathways. They investigated the metabolic composition of seven different gut sections using high-resolution NMR spectroscopy, which returned a comprehensive metabolite overview with a single analytical measurement per sample.
The created list delivers characteristic metabolites, describes metabolite changes along the gut, and highlights the site specificity for selected metabolite pathways. The largest metabolic changes  happened in the cecum, where the microbiome produces microbial metabolites. Furthermore, the evolution of bile acids along the gut was shown and their site-specific conversion was described. A metabolic basis was established for future investigations of metabolic perturbations, which can be introduced by dietary challenges or gene knockouts and provide valuable information for tailored study design and targeted sample collection.
happened in the cecum, where the microbiome produces microbial metabolites. Furthermore, the evolution of bile acids along the gut was shown and their site-specific conversion was described. A metabolic basis was established for future investigations of metabolic perturbations, which can be introduced by dietary challenges or gene knockouts and provide valuable information for tailored study design and targeted sample collection.
These results provide the fundamental analytical and metabolic basis for the investigation of the gut metabolism. Better knowledge of site-specific gastrointestinal metabolism will lead to improved understanding of systemic diseases such as diabetes and obesity and advance dietary, drug intervention and surgical procedure outcomes and guide the way to new therapeutic targets.
Original publication:
Heinzmann SS, Schmitt-Kopplin P. Deep metabotyping of the murine gastrointestinal tract for the visualization of digestion and microbial metabolism. doi: 10.1021/acs.jproteome.5b00034. J Proteome Res. May 1, 2015
Link to the publication:
http://pubs.acs.org/doi/abs/10.1021/acs.jproteome.5b00034
Association between red meat intake and type 2 diabetes risk
Wittenbecher C, Mühlenbruch K, Kröger J, Jacobs S, Kuxhaus O, Floegel A, Fritsche A, Pischon T, Prehn C, Adamski J, Joost HG, Boeing H, Schulze MB. Amino acids, lipid metabolites, and ferritin as potential mediators linking red meat consumption to type 2 diabetes. doi: 10.3945/ajcn.114.099150.
Am J Clin Nutr. June 1, 2015
Habitual red meat consumption is related to a higher risk of type 2 diabetes in observational studies. An interdisciplinary team of DZD scientists at the German Institute of Human Nutrition Potsdam-Rehbrücke, the Helmholtz Zentrum München and the University of Tübingen identified blood metabolites that possibly relate red meat consumption to the occurrence of type 2 diabetes. Analyses were conducted in the European Prospective Investigation into Cancer and Nutrition-Potsdam cohort (n = 27,548), applying a nested case-cohort design (n = 2681, including 688 incident diabetes cases). Six biomarkers (ferritin, glycine, diacyl phosphatidylcholines 36:4 and 38:4, lysophosphatidylcholine 17:0, and hydroxy-sphingomyelin 14:1) in serum samples from baseline were associated with red meat consumption and diabetes risk.
Heme iron intake from red meat is related to higher ferritin levels. The underlying mechanisms that link elevated iron status to the risk of diabetes likely include oxidative stress and modulation of intracellular signaling cascades. Glycine is part of the body’s defense systems against oxidative stress and might ameliorate inflammatory processes. An inverse association of glycine with diabetes risk was previously described. Circulating lipid metabolites partly reflect the nutrient uptake and metabolic processes in the liver. In the literature, several lines of evidence relate a disturbed hepatic lipid metabolism to the pathogenesis of type 2 diabetes.
This is the first study evaluating a large set of metabolites as potential mediators of the association between red meat intake and diabetes risk. The results cannot prove
causality of the observed associations but they hint towards plausible biological pathways linking red meat intake to type 2 diabetes risk. Not least the results provide valuable information for the design and the biomarker assessment of interventional studies.
Original publication:
Wittenbecher C, Mühlenbruch K, Kröger J, Jacobs S, Kuxhaus O, Floegel A, Fritsche A, Pischon T, Prehn C, Adamski J, Joost HG, Boeing H, Schulze MB. Amino acids, lipid metabolites, and ferritin as potential mediators linking red meat consumption to type 2 diabetes. doi: 10.3945/ajcn.114.099150. Am J Clin Nutr. June 1, 2015
Link to the publication:
http://ajcn.nutrition.org/content/101/6/1241.long
Hepatic mitochondrial flexibility lost in patients with steatohepatitis
Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, Herder C, Carstensen M, Krausch M, Knoefel WT, Schlensak M, Roden M. Adaptation of Hepatic Mitochondrial Function in Humans with Non-Alcoholic Fatty Liver Is Lost in Steatohepatitis. doi: 10.1016/j.cmet.2015.04.004,
Cell Metabolism May 5, 2015
DZD scientists showed that obese individuals without steatohepatitis (NASH) have increased mitochondrial respiratory rates compared to lean ones, suggesting hepatic mitochondrial flexibility at early stages of obesity-related insulin resistance. This adaptation is, however, lost in patients with NASH, who have lower maximal respiration, despite higher mitochondrial mass.
These results have been obtained by direct measurement of hepatic mitochondrial content and capacity in humans. The discovered ‘‘hepatic mitochondrial flexibility’’ which is associated with early stages of human obesity could serve as future target for the prevention and treatment of non-alcoholic fatty liver disease (NAFLD).
Original publication:
Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, Herder C, Carstensen M, Krausch M, Knoefel WT, Schlensak M, Roden M. Adaptation of Hepatic Mitochondrial Function in Humans with Non-Alcoholic Fatty Liver Is Lost in Steatohepatitis. doi: 10.1016/j.cmet.2015.04.004, Cell Metabolism May 5, 2015
Link to the publication:
http://www.sciencedirect.com/science/article/pii/S155041311500159X
Successful first step for the prevention of type 1 diabetes
Bonifacio E, Ziegler AG, Klingensmith G, Schober E, Bingley PJ, Rottenkolber M, Theil A, Eugster A, Puff R, Peplow C, Buettner F, Lange K, Hasford J, Achenbach P. Pre-POINT Study Group. Effects of High-Dose Oral Insulin on Immune Responses in Children at High Risk for Type 1 Diabetes: The Pre-POINT Randomized Clinical Trial. doi: 10.1001/jama.2015.2928,
JAMA April 21, 2015
In the international Pre-POINT study, published in the renowned scientific journal JAMA, DZD scientists at the Paul Langerhans Institute Dresden and the Helmholtz Zentrum München achieved a breakthrough in the prevention of type 1 diabetes together with researchers from Vienna, Bristol and Denver (USA): They completed the first step in development of an insulin vaccine successfully.
The study, a double-blind, placebo-controlled, dose-escalation, assessed the immune responses and adverse events associated with orally administered insulin in autoantibody-negative, genetically at-risk children. The immune response to insulin was measured as serum IgG and saliva IgA binding to insulin, and CD4+ T-cell proliferative responses to insulin. In this pilot study of children at high risk for type 1 diabetes, daily oral administration of 67.5 mg of insulin, compared with placebo, resulted in an immune response without hypoglycemia. These findings support the need for a phase 3 trial to determine whether oral insulin can prevent islet autoimmunity and diabetes in such children.
Original publication:
Bonifacio E, Ziegler AG, Klingensmith G, Schober E, Bingley PJ, Rottenkolber M, Theil A, Eugster A, Puff R, Peplow C, Buettner F, Lange K, Hasford J, Achenbach P. Pre-POINT Study Group. Effects of High-Dose Oral Insulin on Immune Responses in Children at High Risk for Type 1 Diabetes: The Pre-POINT Randomized Clinical Trial. doi: 10.1001/jama.2015.2928, JAMA April 21, 2015
Link to the publication:http://jama.jamanetwork.com/article.aspx?articleid=2275446
Innovative approach provides new insights into human metabolism
Wahl S, Vogt S, Stückler F, Krumsiek J, Bartel J, Kacprowski T, Schramm K, Carstensen M, Rathmann W, Roden M, Jourdan C, Kangas AJ, Soininen P, Ala-Korpela M, Nöthlings U, Boeing H, Theis FJ, Meisinger C, Waldenberger M, Suhre K, Homuth G, Gieger C, Kastenmüller G, Illig T, Linseisen J, Peters A, Prokisch H, Herder C, Thorand B, Grallert H. Multi-omic signature of body weight change: results from a population-based cohort study. doi:10.1186/s12916-015-0282-y
BMC Medicine March 9, 2015
Until now there have been few molecular epidemiological studies regarding the effects of weight changes on metabolism in the general population. In a study published in the journal BMC Medicine, DZD scientists at the Helmholtz Zentrum München, the German Diabetes Center Düsseldorf (DDZ) and the German Institute of Human Nutrition Potsdam-Rehbrücke evaluated molecular data of the KORA study*. The applied techniques, metabolomics and transcriptomics, allow the simultaneous determination of a variety of low molecular weight metabolites and gene activities, respectively. This integrated metabolomics and transcriptomics approach improves e.g. the understanding of  molecular mechanisms underlying the association of weight gain with changes in insulin sensitivity.
molecular mechanisms underlying the association of weight gain with changes in insulin sensitivity.
*For more than 20 years the Cooperative Health Research in the Region of Augsburg (KORA) platform has been examining the health of thousands of citizens in Augsburg and environs.
Original publication:
Wahl S, Vogt S, Stückler F, Krumsiek J, Bartel J, Kacprowski T, Schramm K, Carstensen M, Rathmann W, Roden M, Jourdan C, Kangas AJ, Soininen P, Ala-Korpela M, Nöthlings U, Boeing H, Theis FJ, Meisinger C, Waldenberger M, Suhre K, Homuth G, Gieger C, Kastenmüller G, Illig T, Linseisen J, Peters A, Prokisch H, Herder C, Thorand B, Grallert H. Multi-omic signature of body weight change: results from a population-based cohort study. doi:10.1186/s12916-015-0282-y,
BMC Medicine March 9, 2015
Link to the publication:
http://www.biomedcentral.com/1741-7015/13/48/abstract
Cough suppressant improves symptoms of type 2 diabetes
Marquard J., Otter S., Welters A., Stirban A., Fischer A., Eglinger J., Herebian D., Kletke O., Klemen M.S., Stožer A., Wnendt S., Piemonti L., Köhler M., Ferrer J., Thorens B., Schliess F., Rupnik M.S., Heise T., Berggren PO., Klöcker N., Meissner T., Mayatepek E., Eberhard D., Kragl M., Lammert E. Characterization of pancreatic NMDA receptors as possible drug targets for diabetes treatment. doi: 10.1038/nm.3822
Nature Medicine March 16, 2015
Dextromethorphan, an over-the-counter cough suppressant, and its metabolites may improve diabetic complications in mice and humans, according to research published in Nature Medicine. These results suggest a potential adjunct treatment for type 2 diabetes.
Dextromethorphan is an active ingredient, with only a few minor adverse side effects, found in many over-the-counter cough medications and it acts by inhibiting N-Methyl-D-Aspartate (NMDA) receptors. These receptors are expressed in tiny clusters of insulin-producing beta cells in the pancreas, but their physiological role has not been clear.
DZD scientist Eckhard Lammert and colleagues found that genetic deletion of a key part of this class of receptors, or their pharmacological inhibition by drugs such as dextromethorphan, results in more potent glucose-stimulated insulin secretion in a sample of normal mouse and human pancreatic tissue. In addition, the researchers found that dextromethorphan protects pancreatic islets from cell death under certain experimental conditions, which could be of interest to patients with type 1 diabetes.
These results, as well as improved glucose control, were - observed in a mouse model of type 2  diabetes on administration of dextromethorphan. In a small, phase 2a, clinical trial involving 20 volunteers with type 2 diabetes, the authors confirmed that dextromethorphan increases serum insulin concentrations and lowers blood glucose. Long-term clinical studies are now needed to study the benefits of dextromethorphan for patients with diabetes in more depth.
diabetes on administration of dextromethorphan. In a small, phase 2a, clinical trial involving 20 volunteers with type 2 diabetes, the authors confirmed that dextromethorphan increases serum insulin concentrations and lowers blood glucose. Long-term clinical studies are now needed to study the benefits of dextromethorphan for patients with diabetes in more depth.
Original publication:
Marquard J., Otter S., Welters A., Stirban A., Fischer A., Eglinger J., Herebian D., Kletke O., Klemen M.S., Stožer A., Wnendt S., Piemonti L., Köhler M., Ferrer J., Thorens B., Schliess F., Rupnik M.S., Heise T., Berggren PO., Klöcker N., Meissner T., Mayatepek E., Eberhard D., Kragl M., Lammert E. Characterization of pancreatic NMDA receptors as possible drug targets for diabetes treatment. doi: 10.1038/nm.3822
Nature Medicine March 16, 2015
Link to publication:
http://www.nature.com/nm/journal/vaop/ncurrent/full/nm.3822.html





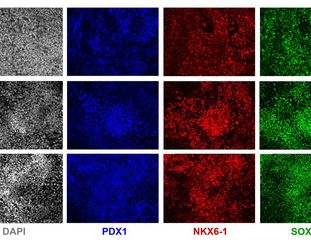
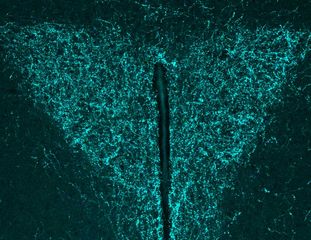
![[Translate to Englisch:] [Translate to Englisch:]](/fileadmin/_processed_/1/1/csm_231130_PubFok-Dez-23_Download_Dev-Cell_1-s2_Ausschnitt_web_0f556bb4d2.jpg)