Tübingen, 19.06.2024
Optimum Protection Against Diabetes: Weight Loss Plus Remission of Prediabetes
People with prediabetes are advised to reduce their weight in order to prevent manifest diabetes. Researchers from the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Munich at the University of Tübingen, a partner in the German Center for Diabetes Research (DZD), together with US colleagues in the renowned “Diabetes Prevention Program (DPP),” have now been able to show for the first time that people achieve the best diabetes protection when they reduce their weight and at the same time normalize blood sugar regulation. In the specialist journal “Diabetologia,” the authors argue that the normalization of blood sugar levels in prediabetes should be included as a therapeutic goal in the guidelines in order to improve the prevention of type 2 diabetes.
Diabetes is widespread and is associated with an increased risk of a number of life-threatening complications such as stroke, heart attack and kidney failure. “In order to prevent the development of the disease, early therapies are already important in the prediabetes stage, a preliminary stage of type 2 diabetes. Our results can be used to change the goals of these early lifestyle interventions in order to reduce the overall development rates of diabetes,” explains first author Reiner Jumpertz-von Schwartzenberg.
Prediabetes drastically increases the risk of diabetes
Prediabetes is diagnosed when there is no manifest type 2 diabetes yet, but the fasting blood sugar is already elevated and glucose tolerance is impaired. To prevent prediabetes from becoming diabetes, affected patients are advised to reduce their weight. US guidelines from the American Diabetes Association (ADA), for example, recommend reducing body weight by at least 7 percent. This recommendation is based on the DPP study.
The research team from the Department of Internal Medicine IV, Diabetology, Endocrinology and Nephrology at the Medical University Hospital of Tübingen, the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Munich in Tübingen and the Phoenix Epidemiology and Clinical Research Branch at the National Institute of Diabetes and Digestive and Kidney Diseases in Phoenix, USA, investigated whether this weight loss is sufficient, or whether it is not better to prevent diabetes by also reducing blood sugar levels such that prediabetes goes into remission.
© Diabetologia / IDM
Prevention through one-year lifestyle intervention
They analyzed data from 480 people with prediabetes who participated in the US Diabetes Prevention Program (DPP) and had lost at least 7 percent of their body weight through a one-year lifestyle intervention. In 114 of them, prediabetes also went into remission during the intervention, meaning that their fasting blood sugar, glucose tolerance and HbA1c had normalized. However, the majority of the 366 study participants had not managed to significantly improve their blood sugar regulation despite successfully losing weight. Their prediabetes was not in remission at the end of the intervention.
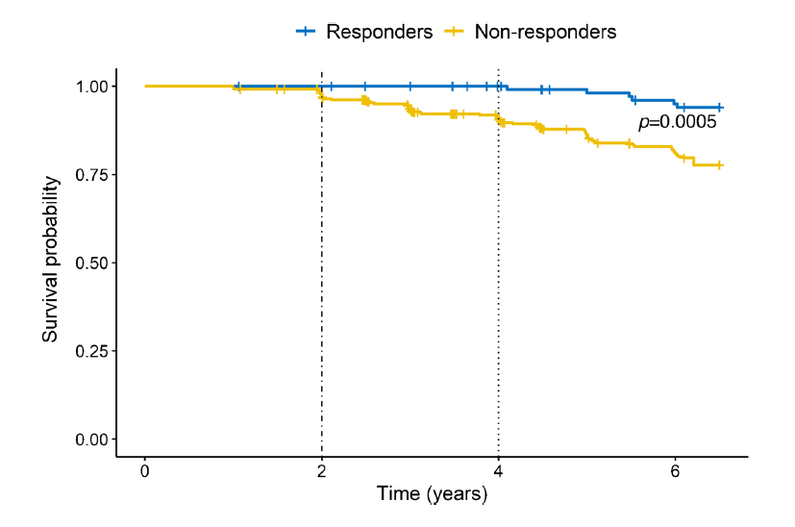
The researchers found that significantly fewer people in the group that had lost weight and achieved prediabetes remission developed manifest diabetes thereafter. The additional remission of prediabetes resulted in a relative risk reduction for the development of diabetes of 76 percent compared to those who had not achieved normalization of their blood sugar levels. The absolute risk reduction was higher than 10%.
“In the group with additional remission of prediabetes, there was even no type 2 diabetes at all in the first 4 years after the lifestyle intervention,” reports last author Andreas Birkenfeld. “In the group that had ‘only’ lost weight, however, some study participants did develop manifest diabetes during that period.”
Jumpertz-von Schwartzenberg and Birkenfeld draw a clear conclusion: “Our results show that remission of prediabetes brings a further significant benefit in addition to weight reduction. We therefore advocate that the goal of prediabetes remission should be included in the objectives of the practice guidelines in order to significantly improve the prevention of type 2 diabetes.”
Original publication:
Reiner Jumpertz-von Schwartzenberg, Elsa Vazquez Arreola, Arvid Sandforth, Robert L. Hanson, Andreas L. Birkenfeld, 2024: Role of weight loss‑induced prediabetes remission in the prevention of type 2 diabetes: time to improve diabetes prevention. Diabetologia, DOI: 10.1007/s00125-024-06178-5
Scientific Contact:
Prof. Dr. med. Andreas Birkenfeld
Phone: +49 (0)7071 29-82735
E-Mail: andreas.birkenfeld(at)med.uni-tuebingen.de
Helmholtz Munich is a leading biomedical research center. Its mission is to develop breakthrough solutions for better health in a rapidly changing world. Interdisciplinary research teams focus on environmentally triggered diseases, especially the therapy and prevention of diabetes, obesity, allergies and chronic lung diseases. With the power of artificial intelligence and bioengineering, the researchers accelerate the translation to patients. Helmholtz Munich has more than 2,500 employees and is headquartered in Munich/Neuherberg. It is a member of the Helmholtz Association, with more than 43,000 employees and 18 research centers the largest scientific organization in Germany. More about Helmholtz Munich (Helmholtz Zentrum München Deutsches Forschungszentrum für Gesundheit und Umwelt GmbH): www.helmholtz-munich.de/en
Founded in 1805, Tübingen University Hospital is one of the leading centers of German university medicine. As one of the 33 university hospitals in Germany, it contributes to the successful combination of high-performance medicine, research and teaching. Well over 400,000 inpatients and outpatients from all over the world benefit annually from this combination of science and practice. The clinics, institutes and centers unite all specialists under one roof. The experts work together across disciplines and offer each patient the best possible treatment based on the latest research findings. Tübingen University Hospital conducts research for better diagnoses, therapies and healing chances; many new treatment methods are clinically tested and applied here. In addition to diabetology, neuroscience, oncology, immunology, infection research and vascular medicine are research priorities in Tübingen. The Department of Diabetology /Endocrinology has been the center of interdisciplinary research over the past 25 years, especially with the participation of surgery, radiology and laboratory medicine. This important discovery of the prediabetes subtypes was only possible due to the interdisciplinary collaboration between the hospital’s various departments. Tübingen University Hospital is a reliable partner in four of the six German Centers for Health Research initiated by the German Federal Government. www.medizin.uni-tuebingen.de
The German Center for Diabetes Research (DZD) is a national association that brings together experts in the field of diabetes research and combines basic research, translational research, epidemiology and clinical applications. The aim is to develop novel strategies for personalized prevention and treatment of diabetes. Members are Helmholtz Munich – German Research Center for Environmental Health, the German Diabetes Center in Düsseldorf, the German Institute of Human Nutrition in Potsdam-Rehbrücke, the Paul Langerhans Institute Dresden of Helmholtz Munich at the University Medical Center Carl Gustav Carus of the TU Dresden and the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Munich at the Eberhard-Karls-University of Tuebingen together with associated partners at the Universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich. www.dzd-ev.de/en
Press contact

Birgit Niesing
niesing(at)dzd-ev.de
+49 (0)89 3187-3971
