Tübingen, 18.07.2024
Prediabetes Remission for Type 2 Diabetes Prevention
Current medical guidelines recommend that people in a preliminary stage of type 2 diabetes lose at least 7 percent of their body weight in order to prevent manifest diabetes. In an article in “Nature Reviews Endocrinology,” diabetes experts Prof. Andreas Birkenfeld and Prof. Viswanathan Mohan advocate glycemic remission (normalization of blood sugar regulation) as a prevention goal for people with prediabetes or a high risk of type 2 diabetes. The article’s claim is supported by numerous international scientists as well as by the DZD’s Prevention Academy.
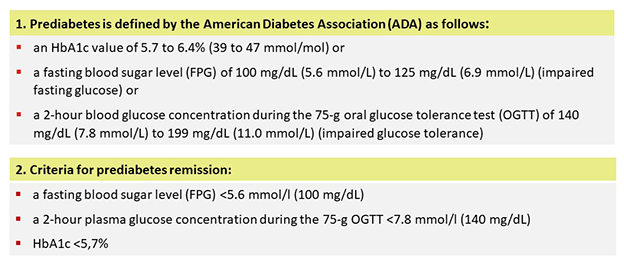
Prediabetes is the greatest risk factor for the development of type 2 diabetes (T2D). In the preliminary stage of diabetes, fasting blood sugar is already elevated and glucose tolerance is impaired (see Box 1). To prevent the development of T2D and damage to blood vessels, lifestyle changes, such as diet and more exercise, are usually used to combat prediabetes. The US guidelines from the American Diabetes Association (ADA) recommend reducing body weight by at least 7%. Nevertheless, the number of diabetes mellitus cases has almost quadrupled since 1980 and the incidence continues to rise—especially in low-income countries. In low- and middle-income countries, the global age-standardized mortality rate for diabetes has also risen by 13% over the past 15 years. According to the two authors, improved strategies are needed to reduce the massive increase in the incidence and prevalence of T2D worldwide and to address the disparities in rates of diabetes mellitus. In addition to weight reduction, they also advocate for incorporating the normalization of blood sugar regulation (prediabetes remission, see Box 1) into diabetes prevention.
Normalizing Blood Sugar Regulation
The concept of “prediabetes remission” was established in analyses of the Prediabetes Lifestyle Intervention Study (PLIS) of the German Center for Diabetes Research (DZD) and the US Diabetes Prevention Program (DPP). The studies showed that in some patients with prediabetes (~40%), weight loss (≥5% of original body weight) led to prediabetes remission. Fasting blood sugar, glucose tolerance and HbA1c levels normalized in this group (see Box 2). Participants who had achieved remission showed a 73% reduced risk of developing T2D even two years after the end of the lifestyle intervention. They also showed reduced markers of kidney damage and better condition of their blood vessels. Some of the participants did not achieve remission despite losing weight and still had prediabetes.
Mechanisms of Prediabetes Remission
Studies have shown that a greater reduction in visceral abdominal fat and improved insulin sensitivity are crucial in achieving prediabetes remission. The authors’ hypothesis is that improving insulin resistance promotes remission from prediabetes to normal glucose regulation. This could indicate that prediabetes remission targets a point in time at which the beta cells are not yet permanently damaged to a clinically relevant extent. This could make prediabetes a window of opportunity to preserve beta cell function in the long term.
Does Prediabetes Remission Reduce the Risk of T2D?
Researchers investigated whether weight loss-induced prediabetes remission is more effective than the currently recommended strategies for preventing type 2 diabetes. They analyzed the data of 480 participants in the Diabetes Prevention Program (DPP) who had prediabetes and had lost at least 7% of their weight through a one-year lifestyle intervention. Blood sugar levels normalized in 114 people (prediabetes remission), while the majority of the 366 participants did not improve their blood glucose regulation. Preliminary results indicate that individuals who achieved prediabetes remission in combination with weight loss of ≥7% reduced their relative risk of diabetes mellitus by 76% over six years compared to weight loss of ≥7% alone.
The authors suggest that remission to normal glucose regulation should be considered in prevention strategies for people with prediabetes. Weight loss plays a decisive role in this regard. The results suggest that people with prediabetes who do not achieve remission after losing at least 7% of their body weight should continue to lose weight until they reach their individual threshold or take other measures.
“We believe that prediabetes remission should be considered in future studies and guidelines as it has the potential to protect beta cell function from the development of type 2 diabetes and possibly reduce the rising incidence and prevalence of type 2 diabetes worldwide,” says Prof. Andreas Birkenfeld. Future studies should clarify whether prediabetes remission can also lead to reduced complication rates.
Publication:
Andreas L. Birkenfeld & Viswanathan Mohan, 2024: Prediabetes remission for type 2 diabetes mellitus prevention. Nature Reviews Endocrinology volume 20, pages441–442
DOI: https://doi.org/10.1038/s41574-024-00996-8
About the Authors:
Prof. Dr. med. Andreas Birkenfeld
Prof. Birkenfeld is head of the Department of Diabetology, Endocrinology and Nephrology at the University Hospital of Tübingen. He is Director of the DZD partner Institute for Diabetes and Metabolism Research (IDM) of Helmholtz Munich at the University Hospital of Tübingen and on the Board of Directors of the German Center for Diabetes Research (DZD).
Prof. Dr. Viswanathan Mohan
The diabetologist and scientist has been active in diabetes research, care and education for over 40 years. He is Chairman of Dr. Mohan's Diabetes Specialities Centre and President and Director of the Madras Diabetes Research Foundation in Chennai, India. He delivered this year's Kelly West Lecture at the ADA.
Scientific Contact:
Prof. Dr. med. Andreas Birkenfeld
Telefon: 07071 29-82735
E-Mail: andreas.birkenfeld(at)med.uni-tuebingen.de
More on this Subject:
Optimum Protection Against Diabetes: Weight Loss Plus Remission of Prediabetes
Press release 19. 06. 2024 about the original publication:
Jumpertz-von Schwartzenberg et al. 2024: Role of weight loss‑induced prediabetes remission in the prevention of type 2 diabetes: time to improve diabetes prevention. Diabetologia, DOI: 10.1007/s00125-024-06178-5
Exercise and Muscle Regulation: Implications for Diabetes and Obesity
Press release 26.09.2023 about the original publication:
Sandforth A, et al. (2023): Mechanisms of weight loss-induced remission in people with prediabetes: A Post-hoc Analysis of the Randomized Controlled Multicenter Prediabetes Lifestyle Intervention Study (PLIS). Lancet Diabetes Endocrinology 2023; https://authors.elsevier.com/a/1hplZ7tNucn7Vs
Helmholtz Munich is a leading biomedical research center. Its mission is to develop breakthrough solutions for better health in a rapidly changing world. Interdisciplinary research teams focus on environmentally triggered diseases, especially the therapy and prevention of diabetes, obesity, allergies and chronic lung diseases. With the power of artificial intelligence and bioengineering, the researchers accelerate the translation to patients. Helmholtz Munich has more than 2,500 employees and is headquartered in Munich/Neuherberg. It is a member of the Helmholtz Association, with more than 43,000 employees and 18 research centers the largest scientific organization in Germany. More about Helmholtz Munich (Helmholtz Zentrum München Deutsches Forschungszentrum für Gesundheit und Umwelt GmbH): www.helmholtz-munich.de/en
Founded in 1805, Tübingen University Hospital is one of the leading centers of German university medicine. As one of the 33 university hospitals in Germany, it contributes to the successful combination of high-performance medicine, research and teaching. Well over 400,000 inpatients and outpatients from all over the world benefit annually from this combination of science and practice. The clinics, institutes and centers unite all specialists under one roof. The experts work together across disciplines and offer each patient the best possible treatment based on the latest research findings. Tübingen University Hospital conducts research for better diagnoses, therapies and healing chances; many new treatment methods are clinically tested and applied here. In addition to diabetology, neuroscience, oncology, immunology, infection research and vascular medicine are research priorities in Tübingen. The Department of Diabetology /Endocrinology has been the center of interdisciplinary research over the past 25 years, especially with the participation of surgery, radiology and laboratory medicine. This important discovery of the prediabetes subtypes was only possible due to the interdisciplinary collaboration between the hospital’s various departments. Tübingen University Hospital is a reliable partner in four of the six German Centers for Health Research initiated by the German Federal Government. www.medizin.uni-tuebingen.de
The German Center for Diabetes Research (DZD) is a national association that brings together experts in the field of diabetes research and combines basic research, translational research, epidemiology and clinical applications. The aim is to develop novel strategies for personalized prevention and treatment of diabetes. Members are Helmholtz Munich – German Research Center for Environmental Health, the German Diabetes Center in Düsseldorf, the German Institute of Human Nutrition in Potsdam-Rehbrücke, the Paul Langerhans Institute Dresden of Helmholtz Munich at the University Medical Center Carl Gustav Carus of the TU Dresden and the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Munich at the Eberhard-Karls-University of Tuebingen together with associated partners at the Universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich. www.dzd-ev.de/en
Press contact

Birgit Niesing
niesing(at)dzd-ev.de
+49 (0)89 3187-3971
