Potsdam-Rehbrücke, 10.09.2020
Epigenetic Changes Precede Onset of Diabetes
Epigenetic* changes in the islets of Langerhans of the pancreas can be detected in patients several years before the diagnosis of type 2 diabetes (T2D). These changes are responsible for the altered methylation activity of specific genes which differs from that in healthy individuals. In humans, 105 such changes have been discovered in blood cells. This was shown in a study by researchers from the DZD/DIfE, which has now been published in the journal ‘Diabetes’. These findings could help to develop diagnostic markers for type 2 diabetes.
Several causes play a role in the development of type 2 diabetes. These include a genetic predisposition, epigenetic factors as well as a diet high in fat and sugar, overweight and lack of exercise. In order to prevent the development of the metabolic disease, it is important to identify people with an increased risk for the metabolic disease at an early stage. Since the development of diabetes can also lead to functional disorders in the islets of Langerhans in the pancreas, researchers from the German Institute of Human Nutrition (DIfE) and the German Center for Diabetes Research (DZD) have investigated whether there are epigenetic changes in the islets of Langerhans that are related to the development of diabetes. Lund University also participated in the study.
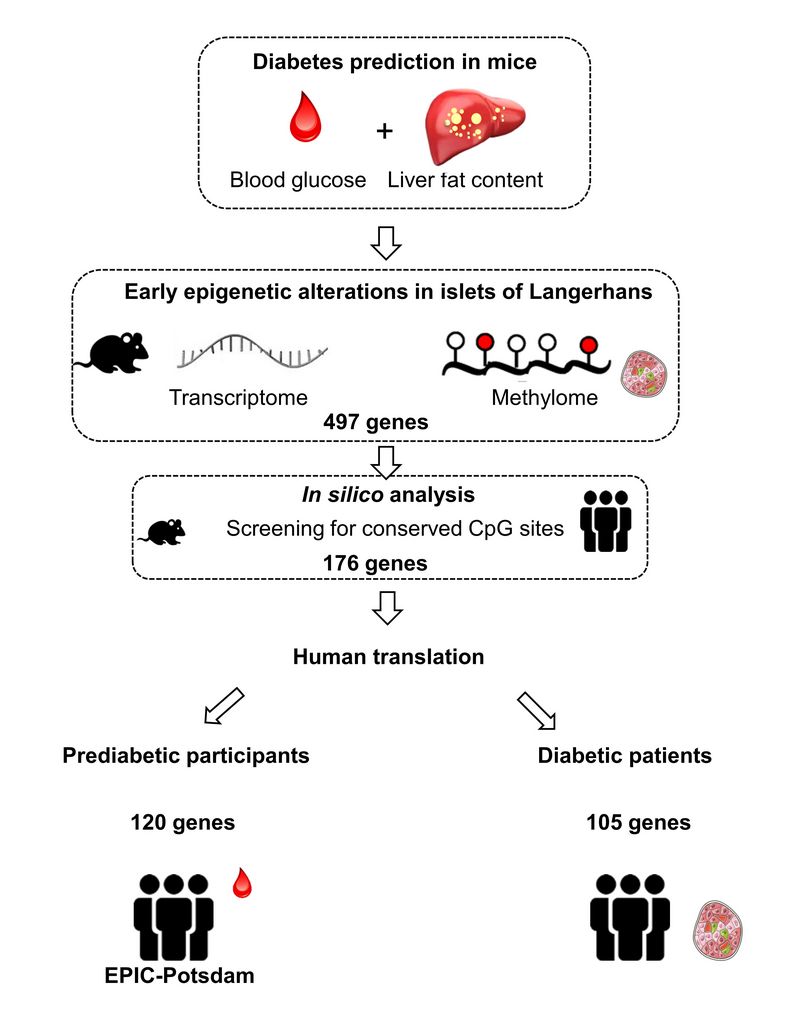
"Our aim was to identify early changes in DNA methylation and the expression pattern in the islets of Langerhans in a diabetes-prone mouse and then to test which of these can also be detected in the blood of humans before diabetes is diagnosed," said Prof. Dr. Annette Schürmann, spokesperson of the DZD and head of the Department of Experimental Diabetology at DIfE, explaining the translational research approach. For this purpose, obese mice were fed a high-calorie diet for five weeks and divided into diabetes-prone and diabetes-resistant animals on the basis of certain criteria (e.g. the liver fat content). The DNA methylations and expression patterns in the islets of Langerhans were determined for both groups. "We were able to identify 497 candidates which differed both in terms of their expression and their DNA methylation," said first author Dr. Meriem Ouni.
The next step was to search for similar epigenetic changes in blood cells of participants in the EPIC-Potsdam study** (270 controls and 270 incident T2D cases on average 3.8 years before diagnosis). The researchers found altered levels of DNA methylation in 105 genes that were associated with the later diagnosis of diabetes. Most of these changes were also found in the islets of Langerhans in type 2 diabetes patients. The researchers assume that most of the alterations in DNA methylation that can be detected in the blood before diagnosis are still present in the islets of Langerhans later in the course of the disease.
“Our broad and translational research approach has identified a number of interesting genes whose expression and altered DNA methylation are associated with the later diagnosis of diabetes," said Schürmann. “In humans, 105 such differences can be detected in blood cells a few years prior to the diabetes diagnosis. This may open up the possibility of using some of these changes as diagnostic markers for type 2 diabetes in the future. "
Next, the researchers want to investigate whether diets or certain drugs can correct unfavorable DNA methylation patterns. They also want to determine whether the identified markers differ in the various diabetes clusters.
* Epigenetics investigates those characteristics of genes that are not revealed by the DNA itself, but by its readability. Epigenetic information is mediated by methyl groups or other biomolecules. Epigenetic marks change the way genes are expressed.They act like a kind of switch in the genome that turns a gene on or off. Current research results suggest that lifestyle can also lead to epigenetic changes.
** EPIC-Potsdam: The European Prospective Investigation into Cancer and Nutrition (EPIC) Potsdam Study is a prospective cohort study. Between 1994 and 1998, 27,548 women and men between the ages of 35 and 65 were recruited. The EPIC Potsdam Study is part of one of the largest long-term studies in the world with a total of around 521,000 study participants from ten European countries. The aim of the study is to investigate the effect of nutrition on the development of cancer and other chronic diseases.
Original publication:
Ouni, M. et al.: Epigenetic Changes in Islets of Langerhans Preceding the Onset of Diabetes. Diabetes 2020;69:1–15 | doi.org/10.2337/db20-0204
Scientific contact:
Prof. Dr. Annette Schürmann
Leiterin Abteilung Experimentelle Diabetologie
German Institute of Human Nutrition Potsdam-Rehbrücke (DIfE)
Arthur-Scheunert-Allee 114-116
14558 Nuthetal
Phone.: +49 (0)33200 88-2368
E-Mail: schuermann(at)dife.de
German Institute of Human Nutrition Potsdam-Rehbrücke (DIfE)
DIfE is a member of the Leibniz Association. It researches the causes of nutrition-related diseases in order to develop new strategies for prevention, therapy and nutritional recommendations. Its research focuses on the causes and consequences of the metabolic syndrome, a combination of obesity (obesity), hypertension (high blood pressure), insulin resistance and fat metabolism disorder, the role of nutrition in healthy aging, and the biological basis of food selection and dietary behavior. DIfE is also a partner of the German Center for Diabetes Research (DZD), which has been funded by the Federal Ministry of Education and research (BMBF) since 2009. www.dife.de/en
German Center for Diabetes Research (DZD)
The German Center for Diabetes Research (DZD) is one of six German Centers for Health Research. It brings together experts in the field of diabetes research and combines basic research, epidemiology and clinical application. By adopting an innovative, integrative approach to research, the DZD aims to make a substantial contribution to the successful, personalized prevention, diagnosis and treatment of diabetes mellitus. The members of the association are Helmholtz Zentrum München - German Research Center for Environmental Health, the German Diabetes Center (DDZ) in Düsseldorf, the German Institute of Human Nutrition (DIfE) in Potsdam-Rehbrücke, the Institute of Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen, and the Paul Langerhans Institute Dresden of Helmholtz Zentrum München at the University Medical Center Carl Gustav Carus of TU Dresden, associated partners at the universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich, and other project partners. www.dzd-ev.de/en
Press contact

Birgit Niesing
niesing(at)dzd-ev.de
+49 (0)89 3187-3971