Dresden, 07.04.2020
Mass or function - PLID scientists provide new puzzle piece for the controversial debate on early type-2 diabetes pathogenesis
Type-2 diabetes (T2D) is characterized by peripheral insulin resistance and insufficient insulin release from pancreatic islet beta cells. However, it is still unclear if the inadequate insulin levels during T2D development are the result of beta cell dysfunction and/or loss of beta cell numbers. Under the lead of Prof. Stephan Speier a collaborative research project involving researchers from the Paul Langerhans Institute Dresden at the Helmholtz Zentrum München and Faculty of Medicine Carl Gustav Carus of TU Dresden, the University Clinic Dresden and King’s College London has now added a critical piece to this controversial debate, by utilizing a novel platform to study the human pancreas in T2D pathogenesis. This unique approach revealed that beta cell function deteriorates early in T2D pathogenesis while beta cell mass in the studied tissue persists. The results of this collaborative work have now been published in ‘Cell Reports’.
The development of T2D is accompanied by metabolic dysregulation which in the early phase is characterized by a modest reduction in glucose tolerance that worsens over time. Crucial for the progression to T2D are inadequate levels of insulin, which adds to the often-observed reduced insulin sensitivity of peripheral tissues. Although T2D pathogenesis has been studied intensively for many years it is still debated whether a loss in the insulin producing beta cells or their dysfunction is the driving force for the reduced insulin levels. This debate is also a consequence of the inability to simultaneously assess mass and function close to the human in vivo situation.
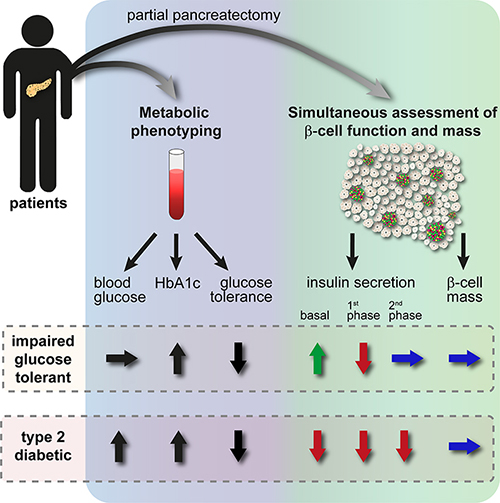
In order to shed light on these questions, the researchers used a novel in situ approach that enables the simultaneous assessment of beta cell mass and function in human tissue. “The combination of our newly established in situ human pancreas tissue slice platform with the thorough metabolic profile of tissue donating cancer patients allowed us for the first time to simultaneously investigate both beta cell mass and function and correlate this to the diseases status of the patients”, explains Prof. Stephan Speier, group leader at the Paul Langerhans Institute Dresden (PLID) and professor at the Institute of Physiology of the TU Dresden. The tissue donors included in this study were part of a larger cohort of patients that had been metabolically phenotyped prior to pancreatectomic surgery, containing non-diabetic (ND), impaired glucose tolerant (IGT) and type 2 diabetic patients, thus representing the full spectrum of T2D development.
The novel approach used within the study employed the freshly resected living tissue to analyze islet function in their preserved organ environment and assess beta cell volume of the investigated tissue afterwards. “After slicing the tissue in 120µm thick sections, we were able to quantify the glucose induced insulin secretion under near physiological conditions from subjects who underwent pancreatectomy in the department of surgery at the University Clinic Dresden. In parallel, we used adjacent slices to explore the detailed 3D cellular morphology which enabled us to normalize insulin output to beta cell volume”, explains lead author Dr. Christian Cohrs from the PLID and the German Center for Diabetes Research.
The research team demonstrated that during the prediabetic state of impaired glucose tolerance beta cells secrete more insulin under basal conditions and show altered release kinetics at stimulating levels of glucose. When the researchers analyzed tissue from type 2 diabetic patients, insulin release dynamics showed further deterioration, leading to an almost total loss in insulin secretion. Interestingly, the number of beta cells in the analyzed tissue remained comparable between all studied groups.
“Our data demonstrate that beta cells exhibit significant functional deterioration and exhaustion already at early stages of T2D pathogenesis, at which subjects exhibit impaired glucose tolerance but are not yet diabetic. Importantly, beta cell numbers in the investigated tissues are maintained”, explains Prof. Speier, “Thus, our results identify beta cell dysfunction as an initial feature of diabetes development and not necessarily as consequence of a preceding loss in beta cell mass”.
“Although the number of studied donor tissues was limited and will require further confirmation in larger cohorts, our results provide novel experimental evidence for an unparalleled depiction of disease pathogenesis, highlighting early beta cell dysfunction as a critical target for the development of successful diabetes prevention and therapy for a major subgroup of T2D patients. It will now be interesting to investigate if these pathogenic processes also apply to other subgroups of T2D”, concludes Prof. Speier.
Original publication:
Cohrs CM, Panzer JK, Drotar DM, Enos SJ, Kipke N, Chen C, Bozsak R, Schöniger E, Ehehalt F, Distler M, Brennand A, Bornstein SR, Weitz J, Solimena M, and Speier S. Dysfunction of Persisting β-Cells is a Key Feature of Early Type 2 Diabetes Pathogenesis. DOI:https://doi.org/10.1016/j.celrep.2020.03.033
The Paul Langerhans Institute of the Helmholtz Zentrum München at the University Hospital Carl Gustav Carus and the Medical Faculty of TU Dresden (PLID) contributes decisively to a better understanding of the mechanisms of the disease and to explore new therapeutic options. The institute is a founding-partner of the German Center for Diabetes Research (DZD e.V.) and has been a satellite institute of the Helmholtz Zentrum München since January 2015. Working in the DZD network allows research projects of a much larger scale, both in the area of basic research through interdisciplinary approaches as well as in the area of clinical studies.
The German Center for Diabetes Research (DZD) is a national association that brings together experts in the field of diabetes research and combines basic research, translational research, epidemiology and clinical applications. The aim is to develop novel strategies for personalized prevention and treatment of diabetes. Members are Helmholtz Zentrum München – German Research Center for Environmental Health, the German Diabetes Center in Düsseldorf, the German Institute of Human Nutrition in Potsdam-Rehbrücke, the Paul Langerhans Institute Dresden of the Helmholtz Zentrum München at the University Medical Center Carl Gustav Carus of the TU Dresden and the Institute for Diabetes Research and Metabolic Diseases of the Helmholtz Zentrum München at the Eberhard-Karls-University of Tuebingen together with associated partners at the Universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich.
Press contact

Birgit Niesing
niesing(at)dzd-ev.de
+49 (0)89 3187-3971