Tübingen, 07.11.2022
Exercise Helps against Insulin Resistance in the Brain
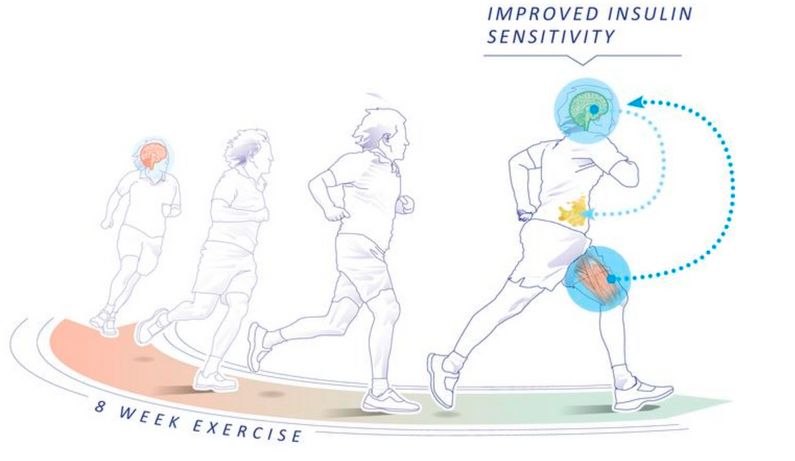
If the brain no longer responds correctly to the hormone insulin (insulin resistance), this also has a negative effect on the metabolism in the body and the regulation of eating behavior. A recent study shows that as little as eight weeks of exercise can help restore the brain's insulin sensitivity in severely overweight adults. This opens up new therapeutic possibilities for reducing obesity and diabetes risk factors in the future. The study by the DZD, Tübingen University Hospital and Helmholtz Munich has now been published in JCI Insight.
The brain has a decisive influence on our eating habits, the metabolism in the body and thus also on body weight. Obese people usually suffer from insulin resistance. If the brain no longer responds to insulin, this also affects regions in the brain that are responsible for the perception of hunger and satiety, as well as for the interaction of motivation, reward, emotions and exercise behavior. It also promotes the accumulation of unhealthy visceral fat and weight regain after a lifestyle intervention 1). So far, there is no established therapy to restore insulin sensitivity in the brain. In a clinical study with 21 overweight and obese adults, researchers have now investigated whether exercise can improve insulin sensitivity in the brain and how the changes affect metabolism and behavior.
Fourteen women and seven men aged 21-59 years with a body mass index* of 27.5 - 45.5 took part in the study. Functional magnetic resonance imaging (MRI) was used to determine insulin sensitivity in the brain before and after eight weeks of monitored endurance training.
Eight weeks of exercise improved insulin sensitivity
The result: the exercise program improved insulin action in the brain to the level of a person with a healthy weight. "The exercise intervention increased the insulin-stimulated activity in brain regions that are responsible, among other things, for the perception of hunger and satiety and for the interaction of motivation, reward, emotion and exercise behavior," said DZD scientist PD Dr. Stephanie Kullmann, who works at the Institute of Diabetes Research and Metabolic Diseases (IDM) of Helmholtz Munich at the University of Tübingen and the Department of Diabetology and Endocrinology at Tübingen University Hospital. The improved insulin sensitivity in the brain had positive effects on the metabolism, the sensation of hunger decreased and the unhealthy visceral fat was reduced.

© IDM
Possible new starting point for therapies against obesity and diabetes
"The study suggests that insulin resistance in the brain may be reversible and could be a viable therapeutic target to restore central nervous system regulation of metabolism and body weight and counteract adverse effects of obesity," said Professor Martin Heni, last author of the study. To verify whether improving brain insulin sensitivity in people at high risk of T2D actually has beneficial effects on metabolism and cognition, further controlled intervention studies are planned. They can also help clarify the underlying mechanisms.
Original publication:
Stephanie Kullmann, … , Cora Weigert, Martin Heni et al.: Exercise restores brain insulin sensitivity in sedentary adults who are overweight and obese. JCI Insight. 2022;7(18):e161498. https://doi.org/10.1172/jci.insight.161498.
*Body Mass Index
The body mass index, or BMI for short, is a formula for evaluating body weight and is used to estimate the body fat percentage. For the calculation of the BMI (body mass index), the body weight is set in relation to body height. The BMI is calculated from the quotient of body weight and height squared (kg/m2). Depending on the level of the value calculated, a distinction is made between the different categories: underweight (below 18.5), normal weight (18.5 to 24.9), overweight (25 to 29.9), extreme overweight (obesity grade 1: 30 to 34. 9), obesity grade 2 (35 to 39.9) and obesity grade 3 (over 40).
1) Kullmann et al. (2020): Brain insulin sensitivity is linked to adiposity and body fat distribution. Nature Communications, DOI: doi.org/10.1038/s41467-020-15686-y
Scientific Contact:
PD Dr. Stephanie Kullmann
Institute of Diabetes Research and Metabolic Diseases (IDM)
of Helmholtz Munich at the University of Tübingen
Otfried Müller Straße 47
72076 Tübingen
E-Mail: stephanie.kullmann(at)med.uni-tuebingen.de
Phone: +49 7071 29 87703
Prof. Martin Heni
Ulm University Hospital – Section for Endocrinology and Diabetology
Albert-Einstein-Allee 23
89081 Ulm
E-Mail: martin.heni(at)uniklinik-ulm.de
Phone: +49 731 500 44505
Founded in 1805, Tübingen University Hospital is one of the leading centers of German university medicine. As one of the 33 university hospitals in Germany, it contributes to the successful combination of high-performance medicine, research and teaching. Well over 400,000 inpatients and outpatients from all over the world benefit annually from this combination of science and practice. The clinics, institutes and centers unite all specialists under one roof. The experts work together across disciplines and offer each patient the best possible treatment based on the latest research findings. Tübingen University Hospital conducts research for better diagnoses, therapies and healing chances; many new treatment methods are clinically tested and applied here. In addition to diabetology, neuroscience, oncology, immunology, infection research and vascular medicine are research priorities in Tübingen. The Department of Diabetology /Endocrinology has been the center of interdisciplinary research over the past 25 years, especially with the participation of surgery, radiology and laboratory medicine. This important discovery of the prediabetes subtypes was only possible due to the interdisciplinary collaboration between the hospital’s various departments. Tübingen University Hospital is a reliable partner in four of the six German Centers for Health Research initiated by the German Federal Government. www.medizin.uni-tuebingen.de
Press contact

Birgit Niesing
niesing(at)dzd-ev.de
+49 (0)89 3187-3971