Dresden, 04.07.2024
Researchers Identify Key Cells for Blood Sugar Control Using Optogenetics
How does our body control blood sugar so precisely? An international team led by Prof. Nikolay Ninov at the Center for Regenerative Therapies Dresden (CRTD), part of Dresden University of Technology, brought us a step closer to the answer. They found a special group of “first responder” cells in the pancreas that are crucial for triggering blood sugar response. Their findings were published in the journal Science Advances.
Our bodies need to keep blood sugar levels just right. Too high or too low can be dangerous. This balance is disturbed in diabetes, leading to serious health issues. Beta cells in the pancreas manage this balance by releasing insulin when blood sugar levels rise. Understanding how beta cells work and coordinate the response to rising blood sugar can ultimately help develop better treatments for diabetes.
Not All Beta Cells Are Equal
“Looking at the pancreas, we wondered if all beta cells are actually equally sensitive to sugar. Previous studies suggested some might be more sensitive than others,” says Prof. Nikolay Ninov, research group leader at the CRTD in Dresden.
To understand the work of the pancreas, the Ninov team turned to zebrafish. This small tropical fish has a pancreas that works similarly to a human one. At the same time, it offers a huge advantage. Researchers can use transparent fish that have no pigment whatsoever and observe the pancreas at work in real-time in the living fish.
The group discovered that a small group of beta cells are more sensitive to sugar levels than the others. These cells respond to glucose quicker than the rest of the cells, so the Ninov team referred to them as “first responder” cells. They initiate the glucose response, which is followed by the remaining “follower cells.”
Hidden Hierarchy in the Pancreas
The team wanted to test if first responders are necessary for the follower cells to respond to glucose. Using transparent fish, the Ninov group took advantage of optogenetics, a modern light-based technology that allows to turn single cells on or off with a beam of light. Turning off the first responder cells lowered the response to the blood sugar of the follower cells. At the same time, when the first responders were selectively activated, the response of the follower cells was enhanced.
“The first responders lie at the top of the beta cell hierarchy when it comes to control of the sugar response. Interestingly, only about 10% of the beta-cells act as first responders. It suggests that this small population of cells serves as a control center for regulating the activity of the rest of the beta cells,” explains Prof. Ninov.”
Unique Traits of First Responder Cells
To find out what makes the first responder cells unique, the researchers compared the gene expression of highly glucose-sensitive beta cells to those that are less sensitive. They found that first responders are involved in vitamin B6 production. The first responder cells express a key enzyme involved in transforming the inactive form of dietary vitamin B6 into the form that is active in the cells.In close collaboration with Prof. Guy Rutter’s team at the University of Montreal, the researchers turned off the vitamin B6 production in both zebrafish and mouse pancreas. The ability of the beta cells to respond to high blood sugar was dramatically reduced in both species.“This indicates that vitamin B6 plays an evolutionarily conserved role in the response to glucose. It is possible that the first responders produce and supply Vitamin B6 to the rest of the beta cells to regulate their activity. Checking whether this indeed is the case is one of our next steps,” says Prof. Ninov.
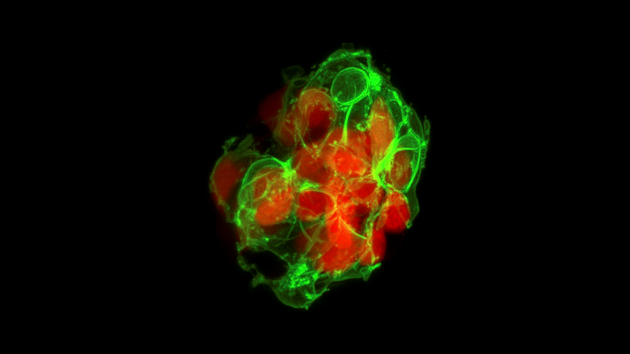
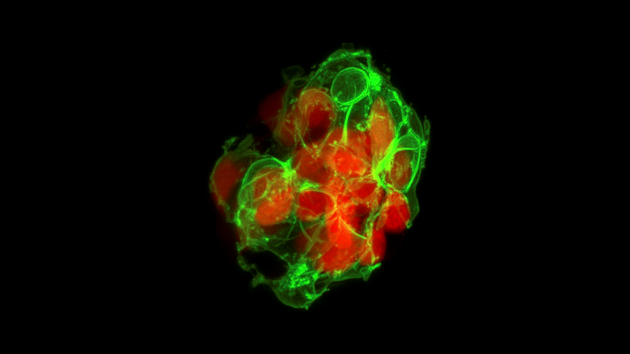
An islet of beta cells in zebrafish pancreas. © Prateek Chawla
Implications for Diabetes Research
“We now know there are specific cells that start the glucose response and that Vitamin B6 is essential for this process," says Prof. Ninov. Vitamin B6 serves as a cofactor for more than a hundred essential enzymes that play critical roles in the cells, ranging from the control of cellular respiration to neurotransmitter production.“There is actually a body of research that shows a correlation between low levels of vitamin B6 and incidence of metabolic disease and type 2 diabetes. We would like to focus more on exploring the link there,” ends Prof. Ninov. Understanding how Vitamin B6 regulates the beta cells in the pancreas could lead to new insights into the pathology of diabetes and ultimately to new treatments.
Original publication:
Luis Fernando Delgadillo-Silva, Emirhan Tasöz, Sumeet Pal Singh, Prateek Chawla, Eleni Georgiadou, Anne Gompf, Guy A. Rutter and Nikolay Ninov: Optogenetic β-cell interrogation in vivo reveals a functional hierarchy directing the Ca2+ response to glucose supported by vitamin B6. Science Advances (June 2024)
Scientific contact:
Prof. Nikolay Ninov
Center for Regenerative Therapies Dresden (CRTD)
Phone: +49 351 458-82314
E-Mail: nikolay.ninov(at)tu-dresden.de
The Technische Universität Dresden (TU Dresden) is one of Germany's niversities of Excellence, esteemed for its exceptional standards in research and teaching spanning diverse fields. The Faculty of Medicine at TU Dresden is dedicated to propelling medical science and healthcare forward through interdisciplinary collaboration and pioneering research. https://www.uniklinikum-dresden.de/en
The Paul Langerhans Institute of Helmholtz Munich at the University Hospital Carl Gustav Carus and the Faculty of Medicine at TU Dresden (PLID) contributes decisively to a better understanding of the mechanisms of the disease and to explore new therapeutic options. The institute is a founding-partner of the German Center for Diabetes Research (DZD e.V.) and has been a satellite institute of Helmholtz Munich since January 2015. Its program comprises research into the pathophysiology of type 1 and type 2 diabetes mellitus. The main focus is on the mechanisms which cause the destruction and/or limited function of pancreatic beta cells and insufficient insulin secretion. In addition, the PLID also plays an outstanding role as only German transplant center for human pancreatic islet cells. https://tu-dresden.de/med/mf/plid
The Center for Regenerative Therapies Dresden (CRTD) of TUD Dresden University of Technology is an academic home for scientists from more than 30 nations. Their mission is to discover the principles of cell and tissue regeneration and leverage this for the recognition, treatment, and reversal of diseases. The CRTD links the bench to the clinic, scientists to clinicians to pool expertise in stem cells, developmental biology, gene-editing, and regeneration towards innovative therapies for neurodegenerative diseases such as Alzheimer's and Parkinson's disease, hematological diseases such as leukemia, metabolic diseases such as diabetes, bone and retina diseases. The CRTD was founded in 2006 as a research center of the German Research Foundation (DFG) and funded until 2018 as a DFG Research Center, as well as a Cluster of Excellence. Since 2019, the CRTD is funded by the TU Dresden and the Free State of Saxony.The CRTD is one of three institutes of the central scientific facility Center for Molecular and Cellular Bioengineering (CMCB) of the TU Dresden.
http://www.tud.de/crtd, http://www.tud/de/cmcb
The German Center for Diabetes Research (DZD) is a national association that brings together experts in the field of diabetes research and combines basic research, translational research, epidemiology and clinical applications. The aim is to develop novel strategies for personalized prevention and treatment of diabetes. Members are Helmholtz Munich – German Research Center for Environmental Health, the German Diabetes Center in Düsseldorf, the German Institute of Human Nutrition in Potsdam-Rehbrücke, the Paul Langerhans Institute Dresden of Helmholtz Munich at the University Medical Center Carl Gustav Carus of the TU Dresden and the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Munich at the Eberhard-Karls-University of Tuebingen together with associated partners at the Universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich. www.dzd-ev.de/en
Press contact

Birgit Niesing
niesing(at)dzd-ev.de
+49 (0)89 3187-3971